Physician stress and burnout was already a major problem prior to the COVID-19 pandemic. In fact, 92% of clinicians in a recent survey have called it a public health crisis. With physician stress and burnout being such a dire problem even in normal times, how much worse is it during this pandemic? In the wake of COVID-19, what can be done to alleviate physician stress and burnout?
In this blog, we’ll look at how the COVID-19 pandemic has worsened burnout, steps hospitals can take to reduce pandemic-related stress and burnout, and some tools that can aid relief efforts.
COVID-19 Effects on Physicians
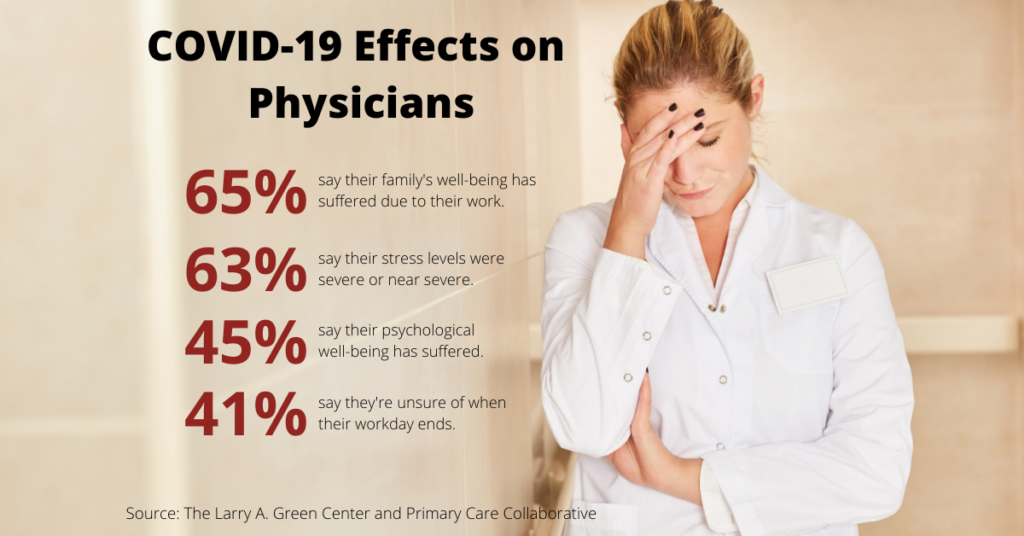
COVID-19 has worsened the effects of stress and burnout on physicians. How much worse are these problems as a result of the pandemic? A survey conducted June 12-15 by Primary Care Collaborative and The Larry A. Green Center examined the effects of COVID-19-related stress and burnout on primary care physicians in 49 states. The survey found that at the height of the pandemic, greater than 80% of physicians were experiencing heightened levels of burnout. Nearly half of respondents stated that both their personal and office burnout was at an all-time high (44 and 48 percent, respectively).
Other results from the survey include:
- 65% said their family’s well-being has also suffered from their work
- 63% said their stress levels were severe or near severe in the four weeks prior to the survey
- 45% said their psychological well-being had suffered
- 41% were unsure of when their workday ends
Physicians are also worried about their patients not getting the care they need. 78% of respondents reported that a majority of their patients have multiple chronic conditions. Despite offering care visits, 48% of respondents said their patients weren’t scheduling them at the time. The lack of visits and other COVID-19 restraints further increased physicians’ stress. 39% reported having to reduce their staff, while a quarter skipped or deferred their own salaries. To make matters worse, 20% of respondents didn’t have access to any known support resources.
Measures to Reduce Pandemic-Related Stress and Burnout
While the Primary Care Collaborative/Larry A. Green Center survey only focused on primary care physicians, those working at hospitals are likely to be just as stressed, if not more. Fortunately, there are measures hospitals can take to alleviate pandemic-related stress and burnout in physicians and other staff.
AMA Recommendations
A recent AMA article lists seven ways to address physicians’ pandemic-related stress and burnout. The seven steps are:
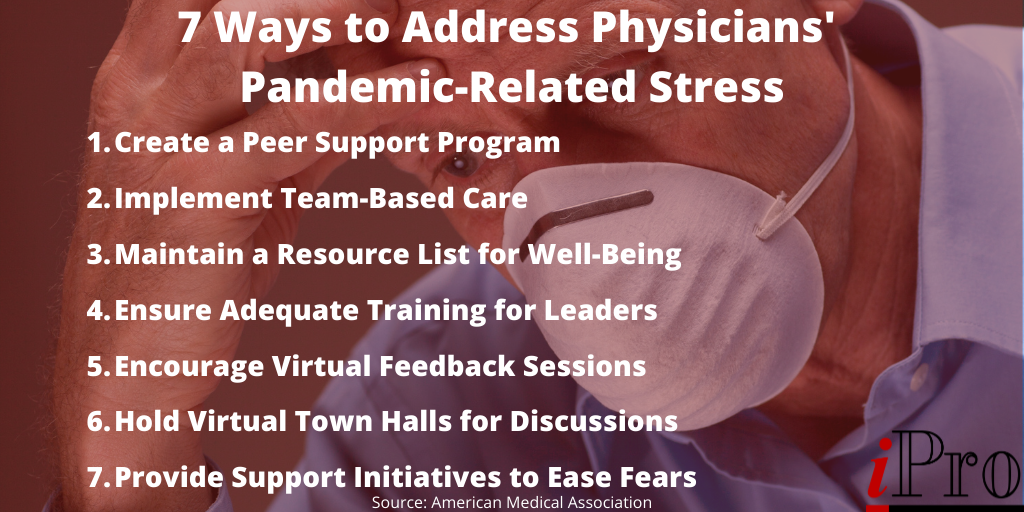
- Create a peer support program – A peer-to-peer support program allows physicians to talk to each other about what they’re experiencing and how to deal with it. The AMA also offers these five steps to building a peer support.
- Implement team-based care – Team-based care helps rebalance and redistribute workloads, which can greatly reduce burnout and stress.
- Maintain a list of resources for well-being – As mentioned in the earlier paragraph, many physicians aren’t aware of resources to support their well-being. You can relieve stress and anxiety among your staff by providing an updated list of resources, such as childcare, transportation, mental health, and more.
- Ensure leaders receive adequate training – Hospital leadership is important in the best of times, and it’s even more important during a pandemic. Ensuring leaders have adequate training goes a long way in the fight to reduce physician stress and burnout. Strong leadership is one of the keys to thriving during the COVID-19 pandemic.
- Encourage virtual feedback sessions – Similar to a peer-to-peer support group, consider implementing virtual feedback sessions, or resilience rounds, to give physicians the opportunity to share what they’re experiencing and how they’re feeling. You can also use the feedback from these sessions to address any pressing needs.
- Hold virtual town halls for discussions – To ensure important communications aren’t lost in the shuffle, hold virtual town halls to inform staff of important news and update them on new protocols. Town halls are also a great opportunity to answer questions your staff may have.
- Provide support initiatives to ease fears – While maintaining a list of support resources is a great way to address physician stress and burnout, going the extra mile by providing some of the resources can have an even greater impact. For instance, consider providing hotel accommodations for staff who are worried about exposing their family to COVID-19.
If you’d like to monitor your staff’s well-being during COVID-19, the AMA is offering two surveys you can use to engage with your staff.
Other Measures to Reduce Stress and Burnout
In addition to the seven steps outline by the American Medical Association, there are some other measures hospitals can take to reduce pandemic-related stress and burnout.
Enhanced Availability of Personal Protective Equipment (PPE)
A June survey of 426 U.S. academic emergency medicine physicians conducted by the Society for Academic Emergency Medicine asked respondents about measures they believe would relieve their stress. Topping the list was the enhanced availability of PPE (96.2% of respondents). It’s no secret that PPE shortages were a major point of stress during the early stages of the pandemic, and ensuring enough PPE is on-hand and accessible through the remainder of the pandemic can help reduce stress and anxiety among physicians and other staff. For tips on improving your supply chain management, check out our recent blog that discusses what several health systems learned from the early stages of the pandemic.
Improved Technology
In addition to the added stress of COVID-19, the technology physicians use on a daily basis is a significant contributor to burnout. A 2019 survey conducted by Spok, a healthcare communications company, found that 90% of clinicians believed “increased and ineffective technology contributes to risk of clinician burnout.” The three technological factors that contributed most to burnout were:
- Burdensome/Increased Workflow (89%)
- Poor Workflow Integration (77%)
- Poor Implementation (61%)
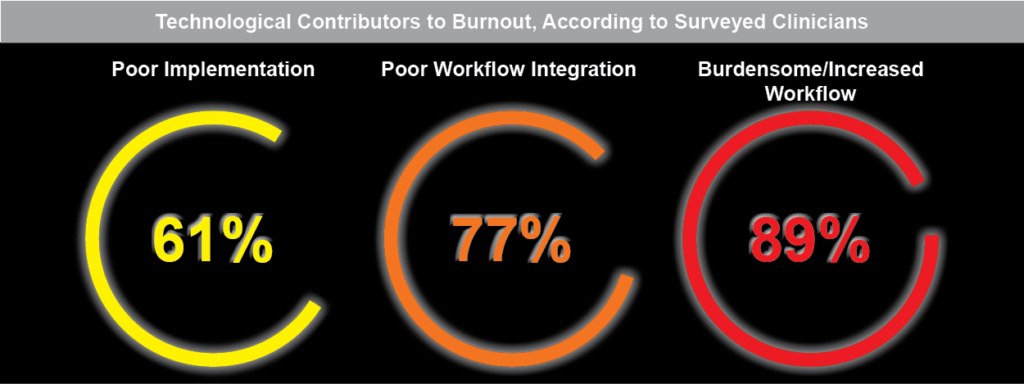
In the next section, we’ll discuss some tools that help overcome these technological contributors to burnout.
Tools to Help Reduce Physician Stress and Burnout
While technology can worsen burnout when it’s ineffective or poorly implemented, it can also reduce stress and burnout when done correctly. There are a variety of solutions that help combat burnout, but the best ones address the number one problem: workflows. As previously discussed, 89% of clinicians reported burdensome/increased workflows contributed to burnout. Technology should always make physicians’ jobs easier. Types of technology that can help streamline and/or reduce workflows include:
- Artificial Intelligence (AI) – AI software can save time by providing predictive analytics and real-time patient insights.
- Automation Software – Automation software saves time and reduces workflows by automating routine tasks, such as automated telephone appointment reminders sent to patients.
- Order Management Software – Order management software streamlines the order process. For instance, our patented ambulatory order management solution with integrated quality decision support mechanism (qCDSM), iOrder, reduces workflows by eliminating faxes, generating an electronic order with all the pertinent information in one place, and reducing errors that result in rescheduled appointments and delayed reimbursements.
- Telehealth – Telehealth can help reduce burnout and stress in a number of ways. Notably, telehealth provides physicians with a way to safely interact with patients, ensuring patients receive the care they need and physicians avoid the risk of being exposed to COVID-19. Effective telehealth solutions, when combined with other software such as AI and voice technology can help save time and reduce workloads.
- Voice Transcription – Voice transcription solutions, such as 3M M*Modal Fluency for Imaging, can save time by eliminating the need for physicians to manually enter notes. As an added bonus, physicians can provide a better patient experience by giving patients more face-time since they aren’t having to look away from the patient to enter their notes.
Working Together to Reduce Physician Stress and Burnout
Physician stress and burnout is bad enough in the best of times. The COVID-19 pandemic has only made it worse. However, following the AMA’s 7 steps to addressing pandemic-related stress outline above and implementing effective technologies that reduce workloads can help fight this growing problem.
You’re not alone in the fight against burnout. At iPro, our vision is to help every client be successful with our software solutions through quality services & support. Our ambulatory order management solution, iOrder, has a host of benefits for providers, physicians, and patients, improving outcomes for all three. By connecting directly to the EMR, iOrder eliminates the need for duplicate data entry. Together with generating electronic orders with complete transparency, this helps reduce the time physicians spend “on hold”, and integrated decision support ensures the right procedure is ordered for the right patient, further reducing stress and improving the patient experience.
To learn more about how we partner with you to achieve your goals every step of the way, check out our interactive partnership lifecycle diagram or contact us today.




