The COVID-19 pandemic is expected to end this year, but many of its effects are sure to linger. Most notably, healthcare burnout, already a serious problem before the pandemic, is showing no signs of going away. In this blog, we’ll look at some of the most recent burnout stats, top contributors to burnout, as well as some tips for fighting healthcare burnout.
Healthcare Burnout Stats
The first step to fighting healthcare burnout is understanding the statistics surrounding it. Important burnout stats to know include:
- How big of a problem it is
- How it affects different specialties in healthcare, and
- Major contributors to burnout
How Serious is Healthcare Burnout?
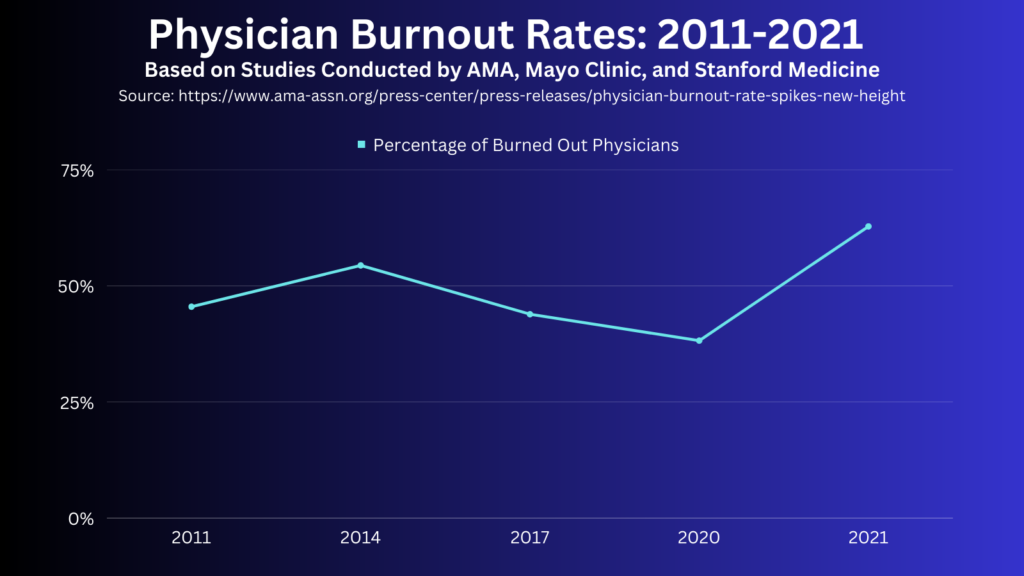
The American Medical Association (AMA), Mayo Clinic, and Stanford Medicine have been surveying physician burnout at regular intervals since 2011. These joint studies were conducted every 3 years from 2011 to 2020, and then again in 2021. The initial study in 2011 saw physician burnout at a worrisome 45.5%. In 2014, this number increased to 54.4%. However, the next two studies saw burnout steadily decline, to 43.9% in 2017 and a low of 38.2% in 2020, the onset of the COVID-19 pandemic. Unfortunately, the pandemic reversed this trend, as evidenced by 62.8% of physicians reporting being burned out in 2021 – the highest burnout has been since the studies began in 2011.
While physician burnout tends to be the main focus, as we’ll see in the next section, burnout is a problem throughout all of healthcare.
Burnout Among Different Specialties
As we saw in the previous section, burnout among physicians is at an all-time high. Healthcare workers in other specialties are feeling the effects as well. Medscape’s latest Nurse Career Satisfaction Report measured burnout among different types of nurses. More than half of nurses in each of the 6 specialties reported feeling at least “somewhat burned out”:
- RN – 68%
- LPN – 68%
- NP – 63%
- CNS – 59%
- CRNA – 56%
- NM – 66%
At least a third of nurses in 4 of the 6 specialties (RN, LPN, NP, & NM) reported being “burned out/very burned out.”
Radiologists are also experiencing high levels of burnout according Medscape’s Radiologist Lifestyle, Happiness & Burnout Report 2023. In the survey, 56% of radiologists said they were burned out (36%), depressed (2%), or both (18%). 44% of radiologists experiencing burnout indicated it had a “strong/severe impact” on their life.
Major Contributors to Healthcare Burnout
Now that we know how big of a problem healthcare burnout is and how it affects different specialties such as physicians, nurses, and radiologists, let’s look at some of the biggest contributors to burnout.
COVID-19
It comes as no surprise that COVID-19 has made healthcare burnout worse. In Medscape’s Physician and Burnout Report 2023, a whopping 79% of physicians stated that the pandemic had affected their work-life happiness at least somewhat in the past year. For 37% of physicians, COVID-19 had a significant impact on their work-life happiness. Radiologists were similarly affected, with 68% reporting COVID-19 at least somewhat affected their work-life happiness (24% significantly). The pandemic has also had a significant impact on nurses’ career satisfaction. 44% or more of CRNA’s, LPN’s, NP’s, NM’s, and RN’s reported decreased career satisfaction due to the pandemic.
Overwork/High Workloads
For physicians, the top contributor to burnout is “too many bureaucratic tasks” yet again according to Medscape’s report. 61% of physicians listed this as a major contributor to burnout, the highest percentage in at least the last three years. “Too many hours at work” was the third biggest contributor to physician burnout, cited by 37% of respondents, up from 34% in 2021 and matching 2020’s level.
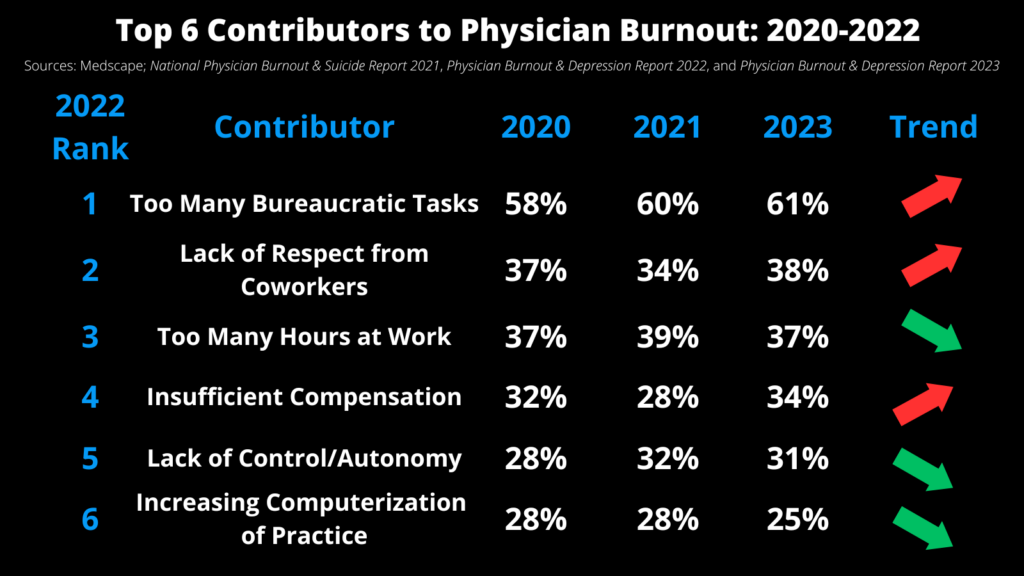
For radiologists, “too many hours at work” was the top contributor to burnout, with 62% of radiologists selecting that choice. While not as big a burnout contributor for radiologists as physicians, “too many bureaucratic tasks” is still a major issue, coming in at number 4 (33%). For both radiologists and physicians, lack of respect from coworkers, lack of control/autonomy, and insufficient compensation were also top five contributors to burnout.
Prior Authorizations
While prior authorizations may fall under the category of “too many bureaucratic tasks”, they’re such a problem that they warrant their own section. A recent survey of physicians by the American Medical Association found that physicians spend an average of 14 hours per week completing prior authorizations – that’s nearly 2 business days! That’s just the time it takes to complete prior authorizations. According to 86% of physicians, the prior authorization process “sometimes, often, or always” leads to more overall utilization of healthcare resources, such as:
- additional office visits
- initial use of less effective therapy due to step therapy requirements
- ER visits, and
- hospitalization
This consumes even more time and contributes even more to burnout. In addition to the prior authorization process’ effect on burnout, 33% of physicians reported that the process has led to a serious adverse event for patients they care for.
What Can Be Done About Healthcare Burnout?
Now that we’ve looked at some of the main contributors to healthcare burnout, let’s look at some solutions to reducing burnout.
Reduce Workloads and Streamline Workflows
Since many of the top contributors to burnout involve time spent working, it’s imperative to reduce workloads and streamline workflows. This not only can reduce burnout, but can improve operational efficiency. Consider automating routine tasks, utilizing AI – such as a clinical decision support mechanism (qCDSM), and outsourcing time-consuming tasks such as prior authorizations.
Ensure Access to Mental Health Care and Support
Burnout takes a serious toll on the mental health of workers. It’s important healthcare workers have access to mental health care and support, such as:
- peer support groups
- mental health support apps
- adequate sick time/paid leave
- courses on coping with stress, burnout, and depression
Check out the AMA’s STEPS Forward® program, a collection of over 70 award-winning online toolkits that help medical teams make changes to their practice, manage stress, prevent burnout, and improve workflows.
Offer Financial Incentives
“Insufficient compensation” is a top burnout contributor for both physicians and radiologists. While many healthcare providers are still cash-strapped 3 years after the onset of the pandemic, it’s worth considering offering financial incentives to reduce burnout and staff turnover.
For more tips on combatting burnout, download a free infographic featuring 18 questions to ask about burnout.
Working Together to Reduce Healthcare Burnout
At iPro Healthcare, we focus on helping healthcare providers improve their workflows to combat burnout, improve patient experience, and maximize ROI. Our ambulatory order management solution, iOrder, accomplishes these goals by:
- Generating an electronic patient order with complete validation and transparency
- Integrating with EHR’s and other third-party solutions for a streamlined workflow
- Improving order accuracy, patient safety, and compliance through integrated clinical decision support
- Enhancing the patient experience and reducing no-shows through SMS-based appointment reminders, links to procedure-specific instruction videos, and facility navigation assistance
- Alleviating the burden of prior authorizations through prior authorization assurance services
- Preventing revenue leakage by strengthening relationships with referring providers
If you’d like to learn more about iOrder and how it can help in your burnout reduction, patient engagement, or revenue cycle initiatives, schedule a free demo today.