Healthcare process improvement teams are always looking for new initiatives to focus on to improve their organization’s efficiency, reputation, and bottom line. Other important initiatives include compliance and patient experience. In this article, we’ll look at four initiatives healthcare process improvement teams should focus on that cover these key areas and some solutions that can help.
1. Improving Prior Authorization Turnaround Time
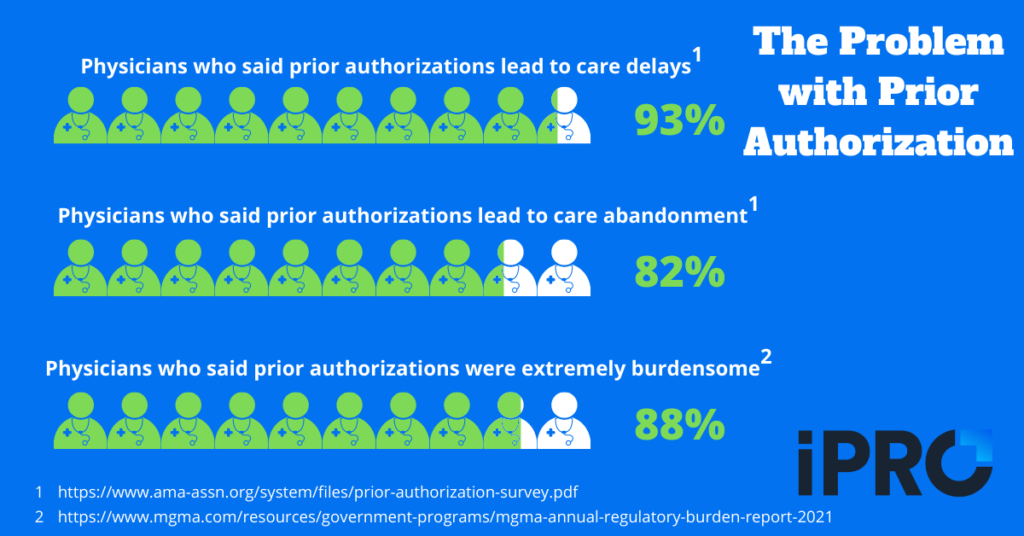
It’s no secret that the prior authorization process is a pain for everyone – patients, physicians, and any other clinical staff involved in the process. Submitting prior authorization requests and following up on them can be time-consuming and tedious for staff. A recent Medical Group Management Association (MGMA) survey found that 88% of physicians reported the prior authorization process was “extremely burdensome”.
The wait for approval can be stressful and frustrating for patients. In fact, in a recent AMA survey, 93% of physicians reported that the prior authorization process can lead to care delays at least sometimes. Even worse, 82% of physicians said the prior authorization process results in patients completely abandoning care at least sometimes. Delayed and abandoned care can lead to serious health consequences for patients, as evidenced by 34% of physicians reporting that prior authorizations had led to a serious adverse event for a patient in their care.
Improving the prior authorization process, and specifically the turnaround time, is a great initiative for healthcare process improvement teams to focus on. A more efficient prior authorization process can:
- reduce clinical burnout
- free up staff to focus on other responsibilities
- improve the patient experience
- reduce no-shows, rescheduling, and care delays/abandonment
That last point leads to our next initiative…
2. Reducing No-Shows, Rescheduling, and Care Delays
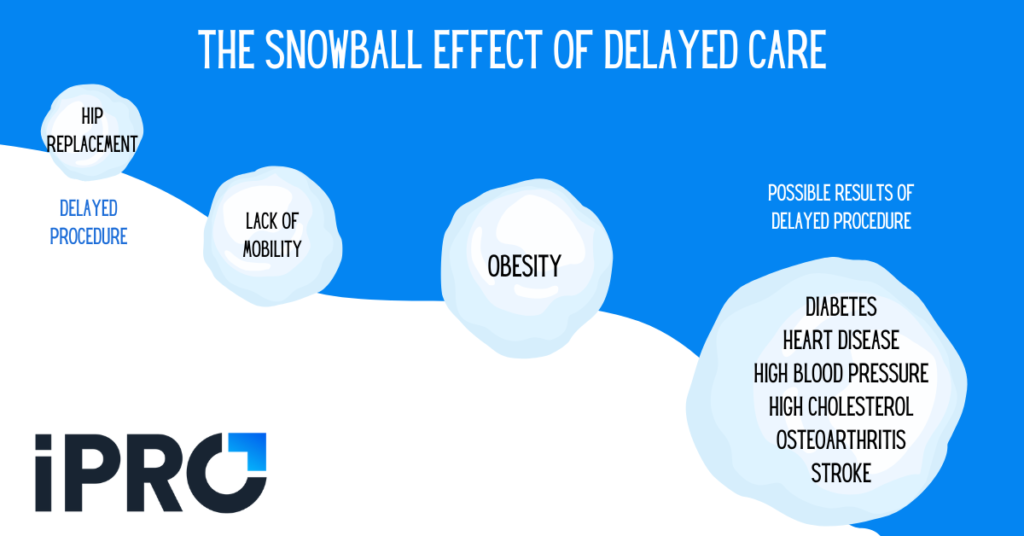
Poor processes can lead to poor patient experiences. Particularly, problems in the scheduling and ambulatory ordering processes can result in the need to reschedule procedures and appointments. This can be due to inaccurate patient or order information, patients arriving without being properly prepared for the exam, or even patients simply forgetting their appointment. No-shows and rescheduling can result in delayed or even abandoned care, leading to higher patient acuity and adverse health consequences. It can also result in revenue leakage for providers.
Healthcare process improvement teams should focus on improving processes that reduce no-shows and rescheduling. These include:
- ambulatory/referral order management
- scheduling
- patient outreach and engagement
Check out these 4 ways to minimize care delays.
3. Implementing Clinical Decision Support
A qualified clinical decision support mechanism, or qCDSM, uses a variety of tools to enhance decision making in the clinical workflow. A qCDSM ensures the correct procedure is ordered for the correct patient through “computable biomedical knowledge, person-specific data, and a reasoning or inferencing mechanism that combines knowledge and data to generate and present helpful information to clinicians as care is being delivered.” Implementing a qCDSM should be a focus for process improvement teams for several reasons.
First, a qCDSM helps improve patient safety and the patient experience by virtually eliminating errors in the ordering process. This reduces the likelihood of adverse events for patients, and it also eliminates the need for rescheduling a procedure due to the wrong procedure being ordered. Clinical decision support also makes physicians’ lives easier by aiding their decision making. A qCDSM offers physicians peace of mind that they’re providing the best care for their patients.
Finally, consulting a qCDSM for Advanced Radiology is a requirement of the Protecting Access to Medicare Act (PAMA). The penalty phase of PAMA has been delayed until further notice, but once implemented, Medicare claims submitted without proof of clinical decision support consultation will be subject to reduced reimbursement and potentially outright denial. Additionally, physicians whose ordering patterns are considered outliers will be subject to prior authorization.
In summary, process improvement teams should focus on implementing a clinical decision support mechanism to improve the patient experience, aid physicians in the ordering process, and maximize reimbursement.
4. Turning Unstructured Data into Structured Data
Many estimates show that 80-90% of data is unstructured, meaning the data doesn’t follow conventional data models. This results in the data not being easily searchable or actionable and requires time-consuming processes to make it actionable. Unstructured data comes in many forms, such as video, text, audio, and images. In healthcare, a major source of unstructured data is faxed medical orders. Unstructured data in faxed medical orders results in various problems, including:
- Errors resulting in denied claims, care delays, patient frustration, and in extreme cases, adverse health outcomes,
- Resource strain from the labor costs and time it takes staff to read documents and/or manually enter data into the EHR, and
- Clinical burnout.
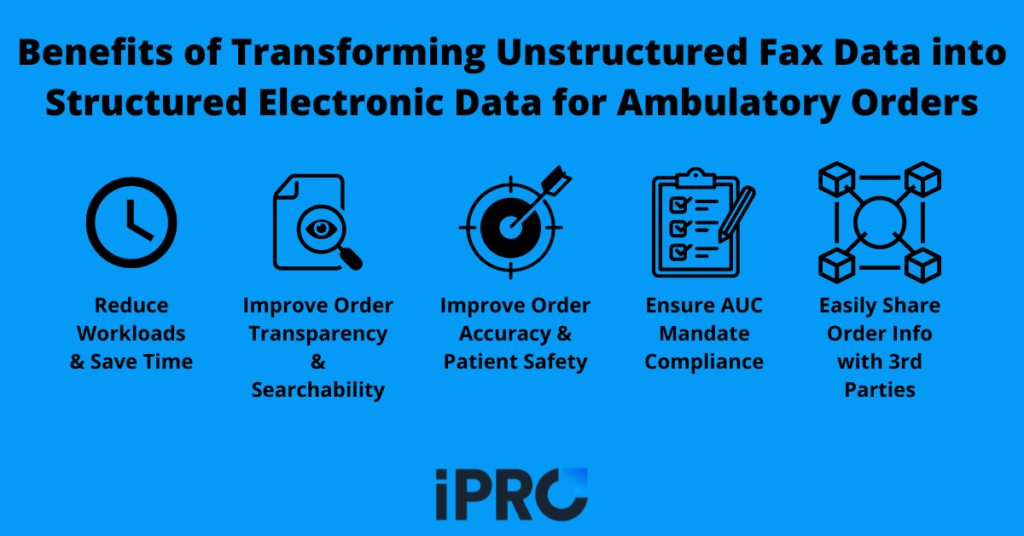
This is why process improvement teams should focus on turning unstructured data into structured data. Structured data is stored in a way that allows for consistency and searchability. Structured data provides benefits such as:
- Reduced labor costs for providers
- More efficient workflows
- Reduced claim denials and care delays
- Reduced burnout and turnover among staff
- Improved patient safety and satisfaction
For a more in depth look at structured data in ambulatory orders, check out our blog on the topic.
Multiple Initiatives, One Solution
Healthcare process improvement teams focus on many initiatives to improve efficiency, patient experience, revenue, and more. The four initiatives we’ve discussed address each of these areas. To recap, the four initiatives are:
- Improving prior authorization turnaround time
- Reducing no-shows, rescheduling, and delayed care
- Implementing clinical decision support
- Turning unstructured data into structured data
At iPro, we offer a single solution to help process improvement teams address all these initiatives and more: iOrder, our flagship referral management solution. With iOrder, referring physicians can generate an electronic patient order with complete transparency. Unlike unstructured data in faxed orders, electronic orders through iOrder are complete with structured, actionable data and are completely interoperable with EHR’s. iOrder also provides order validation, and its integrated qCDSM ensures compliance, patient safety, and maximized reimbursement. A third-party prior authorization integration also removes the burden of prior authorizations from clinical staff and improves turnaround time. Coupled with iOrder’s text message notifications and appointment reminders, procedure-specific instruction videos, and facility navigation assistance, iOrder reduces no-shows, rescheduling, and delayed care.
If your process improvement team is considering any or all of the initiatives we’ve discussed in this article, iOrder is the tool they need.
Watch the video below for a brief overview of iOrder, or schedule a free live demo today!




