It seems like a new problem arises in healthcare everyday. Healthcare workers and leaders must stay on their toes and be able to quickly adapt to new challenges as they pop up. As we start the new year, let’s take a look at four of the biggest problems in healthcare and tips for addressing them:
- Consistent quality of care
- Rising expenditures
- Shortages and inefficiencies
- Administrative waste
Consistent Quality of Care
One of the biggest problems in healthcare is the consistent quality of care. The pandemic not only directly harmed patients by making them sick, but it also indirectly harmed them by forcing them to delay treatment. While the pandemic has subsided and things have largely returned to normal, delayed care has resulted in an uptick in otherwise preventable health issues in patients. Now more than ever is it important for providers to ensure they’re offering quality care consistently.
Some keys to providing quality care consistently include:
Effective Communication
It’s important for care teams, both internal and inter-facility, to communicate quickly and effectively. This ensures patients receive the care they need when they need it. Communicating with patients themselves and their families is equally important. Patients who have a clear understanding of their treatment are likely to be more satisfied and feel less anxiety.
Innovative Tech
Investing in up-to-date and innovative tech is also critical to providing consistent quality care. Outdated tech can lead to inefficient processes, which could result in staff burnout, errors, care delays, and dissatisfied patients. Providers should focus on investing in tech that improves efficiency and accuracy, as well as tech that makes patients’ and providers’ lives easier.
Minimizing Care Delays
Delayed care can lead to a snowball effect of negative outcomes for patients.
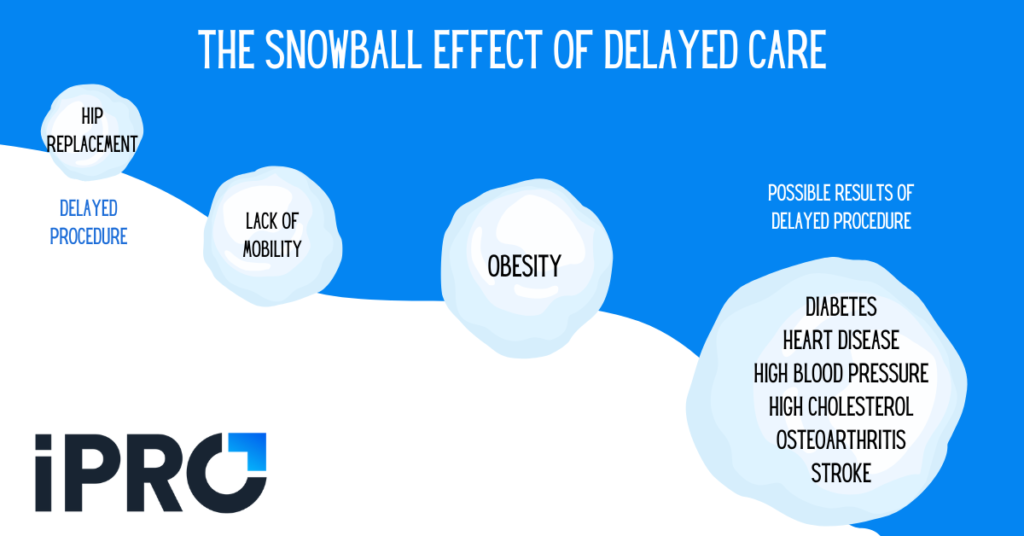
As mentioned earlier, the COVID-19 pandemic led to a strong uptick in care delays. Even as the pandemic subsides, care delays still happen for a variety of reasons, including:
- Prior authorization issues and/or claim denials
- Clerical errors/inaccurate order information
- Improperly prepared patients
To minimize care delays, providers should improve efficiencies in the order and claims processes as well as improve their patient engagement initiatives.
Reducing Staff Burnout and Turnover
Healthcare staff’s interactions with patients is arguably the most important aspect of the quality of care they receive. From the receptionist to the physician, friendly, attentive staff are a must. With burnout a major problem in healthcare, it’s essential for healthcare leaders to take measures to mitigate it. In the next section, we’ll take a more in depth look at staffing issues.
For more ideas on improving patient experience, check out this Becker’s Healthcare article featuring strategies from 5 health system leaders.
Shortages and Inefficiencies
While 2022 saw monthly healthcare job growth roughly 4.5 times higher than 2021, staffing shortages are still a concern in the industry. An October 2022 survey found that 85% of healthcare providers are experiencing a shortage of allied healthcare professionals, including radiologic technologists, physical therapists, and lab technicians. According to the respondents, the biggest challenges in recruiting workers are:
- The current labor shortage (80%)
- Longer times to fill positions (71%), and
- Burnout (46%)
Staffing shortages can lead to inefficient processes, increased burnout among staff, errors, patient safety issues, and more. Addressing burnout can go a long way in staff retention. Improving efficiency by streamlining workflows and reducing workloads through automation can help reduce burnout. These more efficient processes also help improve the quality of care patients receive.
In addition to reducing burnout, a recent Becker’s Healthcare article recommends these five strategies for hiring healthcare workers:
- Offering “gig” shifts for part-time and full-time healthcare workers
- Recruiting former employees that left during the pandemic
- Hiring high school students as support staff
- Promoting open positions on billboards
- Using recruiting and staffing apps that utilize AI to match top candidates with open positions
If you’d like to start a conversation about burnout at your facility, download our free infographic featuring Harvard Business Review’s 18 Questions to Ask about Burnout.
Rising Expenditures
Another major problem in healthcare is rising expenditures. An October 2022 report by Strata found that YTD expenses per adjusted discharge are up 25.9% and 9.6% compared to 2019 and 2021 respectively. Revenue per adjusted discharge is only up 19.3% and 2.6% compared to 2019 and 2021 respectively. A July 2022 survey by the MGMA (Medical Group Management Association) echoes these findings with 90% of medical practices reporting costs rising faster than revenues in 2022.
Not surprisingly, both reports found that staffing and labor costs were the most common area of rising costs. As we mentioned in the previous section, staff turnover has been a major problem in healthcare for several years now, exacerbated by the pandemic. To retain and attract top talent, healthcare providers have resorted to paying higher salaries and bonuses. The Strata report found that the median labor expense direct cost per encounter is up 54.3% compared to 2019 for short term acute care hospitals. One practice leader told MGMA their practice had budgeted for an 8% cost-of-living raise for all staff but ended up paying about 12%.
Other major sources of rising costs reported in the MGMA survey include:
- Lab supplies
- Drugs
- Utilities
- Malpractice insurance rates
With expenses on the rise, healthcare leaders must be more conscious of where their money is being spent. While implementing new technology is critical for health systems to offer a better experience for both staff and patients, leaders must prioritize tech with higher ROI to offset rising expenditures.
Administrative Waste
The final healthcare problem we’ll discuss is administrative waste. According to a recent Health Affairs report, administrative spending accounts for 15 to 30 percent of U.S. medical spending. Administrative spending is typically broken down into two broad categories:
- billing- and insurance-related expenses – claims management, clinical documentation and coding, and prior authorization, and
- non-billing- and insurance-related expenses – general business overhead such as quality assurance, excise taxes and profits, and credentialing costs.
While most administrative spending is necessary, it’s estimated that half of administrative spending is wasteful. This means that 7.5 to 15 percent of medical spending is unnecessary, often due to inefficient processes or regulations.
While an overhaul of government regulations is needed to eliminate administrative waste completely, there are some measures providers can take to reduce waste. Improving efficiencies in the prior authorization and coding processes is a great way to curb administrative costs. For example, healthcare providers may be able to save money by outsourcing their prior authorization costs to a third-party specialist, as opposed to the labor costs of full-time prior authorization staff. Investing in software that improves coding accuracy and eliminates code mismatches can reduce costly errors in the coding process.
Partnering for Success
With all the problems in healthcare, it’s important for healthcare leaders to identify and focus on the ones that have the biggest impact on their organization. While each organization faces different challenges, four of the biggest problems in healthcare are:
- Consistent quality of care
- Shortages and inefficiencies
- Rising expenditures
- Administrative waste
At iPro, we’ve been helping clients overcome problems in healthcare for 25 years. Our award-winning referral order management solution, iOrder, addresses all the problems we’ve discussed. By generating an electronic order with complete transparency and validation, iOrder:
- eliminates faxes and lost orders
- streamlines workflows
- improves order accuracy and eliminates coding errors
- reduces workloads
iOrder also helps minimize care delays and improve the patient experience by sending patients automated appointment reminders, procedure-specific instruction videos, and navigation assistance via text. Integrations such as a qualified clinical decision support mechanism (qCDSM) and prior authorization assurance services can also minimize care delays and reduce burnout among staff.
If you’d like to learn more about iOrder, request a free live demo today.




