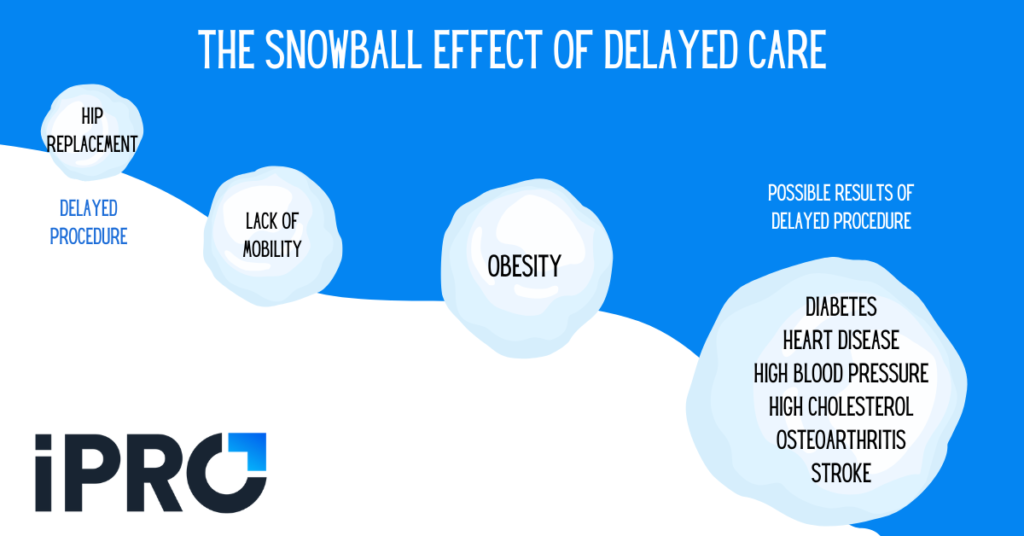
When insurance claims are denied or delayed, providers and patients both feel the pain. Providers miss out on much needed revenue. Denied or delayed claims can lead to care delays, already a problem due to the pandemic, which can adversely affect patients’ health. In fact, care delays can turn into outright abandoned care or lead to a snowball effect of health problems down the road. A recent report by the American Hospital Association also links delayed care to increased patient acuity.
In this blog, we’ll take a look at four ways providers can minimize outpatient claim denials and care delays, thus maximizing reimbursements and ensuring the best health outcomes for patients.
Improving Processes, Engaging Patients
Addressing problems in the ambulatory order process should be the primary focus in minimizing claim denials and care delays. Particularly, providers should focus on improving three key areas of the ambulatory order process:
- Order validation and transparency
- Insurance prior authorizations
- CMS program compliance
Ensuring efficiency and accuracy in these three areas helps minimize claim denials, leading to higher reimbursement rates and fewer care delays. However, a fourth factor should be addressed to further minimize the chance of care delay or abandonment: patient engagement. Even if your ambulatory department is dotting all the I’s and crossing all the T’s in the order and claim process, gaps in patient outreach and engagement can lead to rescheduled or even completely canceled appointments. Read on to learn more about addressing all four of these factors.
1. Ensure Ambulatory Order Validation and Transparency
The first step to minimizing outpatient care delays and claim denials is to ensure ambulatory orders are validated and completely transparent. If information on an outpatient order isn’t validated, insurers may deny coverage due to inaccurate information. Beyond insurance implications, inaccurate information can lead to unprepared patients or staff. For example, if a patient exceeds the weight limit of an MRI table and this issue isn’t caught when submitting the order, an awkward and frustrating situation may arise on the day of the exam when they’re told the MRI can’t be performed.
Similarly, order transparency is critical to minimizing care delays. Order transparency means all parties involved in an outpatient order – patient, referring physician, and clinical staff – have access to the order’s status at all times. This helps ensure orders aren’t missed or overlooked and that any modifications to an order are communicated to applicable parties.
An ambulatory order management platform like iOrder can provide order validation and transparency.
2. Streamline Your Prior Authorizations Process
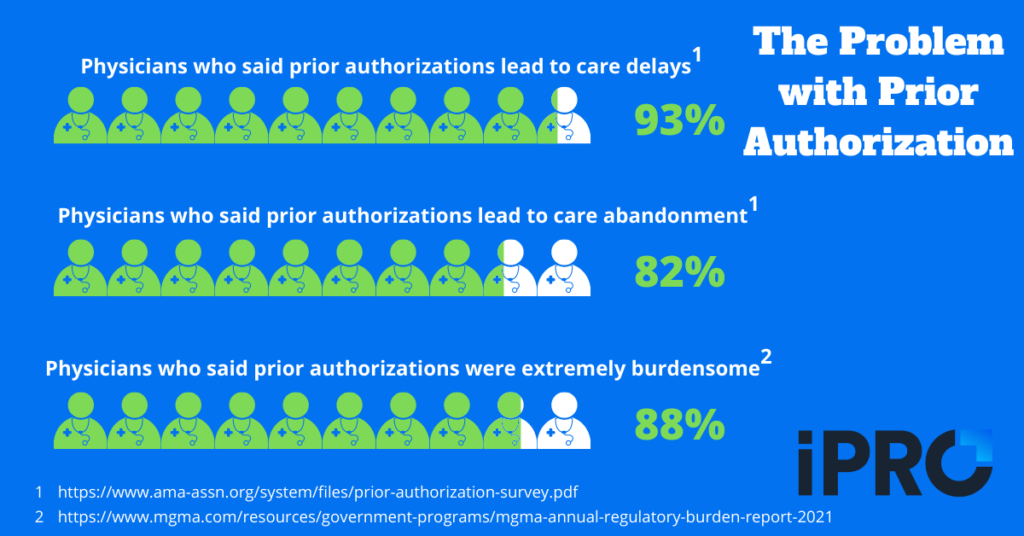
The second step to minimizing claim denials and care delays is to streamline your prior authorizations process. According to a 2021 American Medical Association survey, 93% of physicians surveyed said that prior authorizations lead to care delays at least “sometimes”, with 56% reporting care delays “often” or “always”. Furthermore, 82% said issues related to the prior authorization process can lead to abandoned care, with 24% reporting this happens often.
Ensuring prior authorizations are completed in a timely manner so as to prevent care delays can be very time-consuming. In fact, in the Medical Group Management Association’s (MGMA) October 2021 Annual Regulatory Burden Report, prior authorizations were the most burdensome regulation with 88% of physicians saying they were “extremely burdensome”. Even when clinicians submit accurate information for prior authorization, insurers may drag their feet or outright deny coverage, an illegal practice that has led the American Hospital Association to call on the DOJ to conduct False Claim Act investigations into private insurers.
A great way to improve prior authorization turnaround time without overworking clinical staff is to outsource your prior authorizations process. Prior authorization specialists, such as AuthNet, handle all the work and ensure a quick turnaround. This frees up your own staff to focus on other tasks and ensures prior authorizations don’t delay patient care.
Learn how improving your prior authorization turnaround time can help you build a better brand in our recent blog.
3. Implement Clinical Decision Support
Another way to minimize claim denials is to ensure compliance with CMS’ Appropriate Use Criteria (AUC) mandate. Ensuring compliance is difficult at the best of times for healthcare providers, but even more so given the recent staffing issues. Implementing a Clinical Decision Support Mechanism, or qCDSM, not only makes physicians’ jobs easier, it also ensures AUC compliance.
Delayed for several years due to COVID-19, the penalty phase of the AUC mandate is set to begin January 1st, 2023. Any Medicare claims submitted by radiologists or imaging providers without proof of qCDSM consultation after this date will be not be paid. Ordering physicians themselves won’t face financial penalties for submitting orders without proof of qCDSM consultation, placing the onus on the hospitals or imaging providers performing the exam. Providing referring providers with the proper qCDSM tools and education on the AUC mandate will be critical to minimizing claim denials. Implementing an order management system with integrated qCDSM is a great way to do this.
4. Keep Patients Engaged
The first three recommendations for minimizing claim denials and care delays focused on the order and claims processes. Our final recommendation focuses on the patient. Ambulatory order accuracy and compliance won’t matter for much if patients aren’t engaged. Gaps in patient engagement can lead to delayed or abandoned care in a number of ways, such as:
- Patients forgetting their appointments
- Patients arriving late due to navigation difficulties
- Patients showing up unprepared (not following instructions, etc.)
Implementing patient engagement measures can help eliminate these issues and care delays. Consider implementing the following to improve your patient engagement initiatives:
- Automated appointment reminders via text/call
- Links to GPS/navigation assistance
- Links to procedure specific instructions to ensure patients are properly prepared
Implementing these patient engagement tactics not only helps prevent care delays, it also helps improve your ambulatory outreach.
Your All-in-One Solution for Minimizing Care Delays: iOrder
So far, we’ve covered four tactics to minimize claim denials and care delays:
- Ensuring ambulatory order validation and transparency
- Streamlining the prior authorization process
- Implementing Clinical Decision Support
- Keeping patients engaged
At iPro, our iOrder ambulatory order management platform is an all-in-one solution for implementing all four of these tactics. First and foremost, iOrder generates an electronic order with complete validation and transparency. This ensures order information is accurate and accessible every step of the way. Second, our integration with AuthNet removes the burden of prior authorizations from your clinical staff and ensures timely completion of prior authorizations.
We also offer integrated Clinical Decision Support to further ensure order accuracy, patient safety, and AUC compliance. This means your referring providers have the necessary tools to submit proof of qCDSM consultations with every order, ensuring Medicare claims are paid and care isn’t delayed due to red tape. Finally, iOrder bolsters your patient engagement initiatives with automated appointment reminders, facility navigation assistance, and links to procedure-specific instruction videos, all via text.
Watch the video below for a brief overview of how iOrder works, and schedule a free live demo to learn more!




