The Centers for Medicare and Medicaid Services, or CMS, is one of the premiere healthcare regulation agencies in the U.S. While CMS recently announced an indefinite delay of the penalty phase of their Appropriate Use Criteria (AUC) mandate, healthcare providers should be aware of another important program: CMS quality measures.
In this article, we’ll discuss what CMS quality measures are, how you can improve your scores, and how we can help along the way.
CMS Quality Measures 101
So, what exactly are CMS quality measures? According to CMS themselves,
Quality measures are tools that help us measure or quantify healthcare processes, outcomes, patient perceptions, and organizational structure and/or systems that are associated with the ability to provide high-quality health care and/or that relate to one or more quality goals for health care. These goals include: effective, safe, efficient, patient-centered, equitable, and timely care.
– Centers for Medicare and Medicaid Services
CMS uses these quality measures in a variety of ways, including:
- Quality improvement initiatives
- Public reporting, and
- Pay-for-reporting programs for specific healthcare providers
For healthcare providers, the pay-for-reporting program is arguably the most important aspect of the CMS quality measures. Specifically, the Hospital Outpatient Quality Reporting Program (Hospital OQR Program) requires hospitals meet administrative, data collection & submission, validation, and publication requirements. If these requirements aren’t met, a 2 percentage point reduction in payment will be assessed. This may not seem like much, but it can add up over time.
View a list of CMS quality measures here.
Ways to Improve Your Ratings for CMS Quality Measures
CMS recently released their star ratings for 2022. The star ratings range from 1 to 5, with 1 being the lowest score and 5 being the highest. This most recent round of ratings of 3,093 hospitals breaks down as follows:
- 429 (14%) of hospitals received a perfect 5-star rating
- 890 (29%) of hospitals received a 4-star rating
- 890 (29%) of hospitals received a 3-star rating
- 693 (22%) of hospitals received a 2-star rating
- 191 (6%) of hospitals received the lowest rating of 1 star
The majority of hospitals (1,780 or 58%) received 4 and 3-star ratings, indicating a strong foundation for quality healthcare but room for improvement. With that in mind, let’s look at a few ways hospitals can improve their star ratings.
Establish a Quality Improvement Program
When striving to improve your quality star rating, it’s important to have a strategy in place. Consider establishing a quality improvement program to plan, guide, track, and analyze your quality improvement efforts. Your quality improvement program should include:
- Appointing a committee to oversee the initiative and make changes when necessary
- Identifying areas of improvement via self-assessment, patient surveys, and/or third party quality audits
- Establishing realistic quality improvement goals and procedures for tracking them
- Executing the plan of action
- Staying up-to-date on the latest CMS quality initiatives
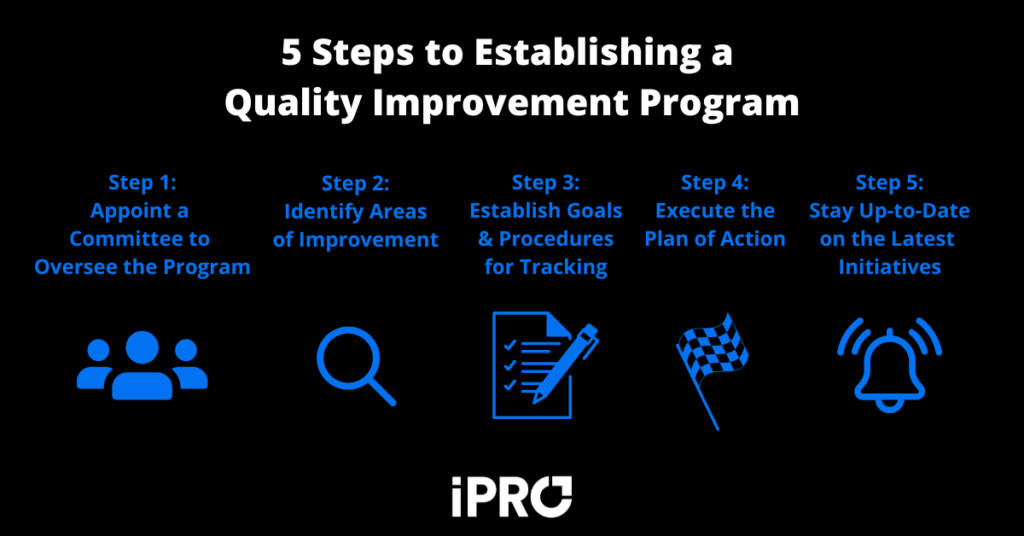
With a quality improvement program in place, your organization will have a better chance of attaining your goals and improving your star rating.
Attract and Retain the Right Staff
A quality improvement program can only be successful with the right staff. The pandemic put a major strain on healthcare workers, creating staffing challenges for hospitals. For example, a recent survey of registered nurses found that a whopping 67% plan to leave their position within the next 3 years. Hospitals should strive to keep employees happy and address issues they face. Employees’ health and wellbeing is just as important as patients’.
Improving the quality of the work environment can also help improve your CMS quality measures by achieving organizational buy-in. A happy and healthy workforce is less prone to making errors and more apt to provide a great patient experience. Additionally, a recent Harvard Business Review article discusses how offering a “career portfolio” which focuses on unlocking skills and connections for employees may be a better retention technique than the traditional “career ladder” approach.
For an in depth look on how tech can help combat staffing issues, read our blog on the topic.
Invest in Technology that Addresses CMS Quality Measures
The final strategy for improving your CMS quality measures is to implement tech solutions that address the measures. Given that there are over 1,000 CMS quality measures, the tech you employ should depend on the services you provide and the areas in which you need to improve the most. Generally, tech that does the following will help your quality improvement efforts:
- Ensures patient safety
- Minimizes care delays/abandonment & readmission rates
- Reduces errors
- Streamlines workflows and improves efficiency
A variety of solutions are available to address CMS quality measures, from order management software to AI-based solutions. In the next section, we’ll take a look at how our flagship solution, iOrder, can help improve your star ratings in specific categories.
Align Your Quality Stars with iOrder
At iPro, we’ve been helping healthcare providers improve their processes for over 20 years. When it comes to improving your CMS quality star ratings, our referral management solution, iOrder, can help in a number of ways. Let’s look at some specific CMS quality measures and how iOrder addresses each one.
OP-8: MRI Lumbar Spine for Low Back Pain
CMS Quality Measure OP-8: MRI lumbar spine for low back pain is the percentage of patients who underwent an MRI scan of the lumbar spine with a diagnosis of low back pain without claims-based antecedent of conservative therapy. A recent Northeastern University study shows that doctors are often pressured to order unnecessary MRI’s to boost hospitals’ bottom lines. To combat this challenge, iOrder includes Clinical Decision Support and validation of medical appropriateness which allows physicians to order correctly every time, shedding light on potentially unnecessary MRI exams.
OP-10: Abdomen CT Use of Contrast Material
CMS Quality Measure OP-10: Abdomen CT use of contrast material measures the proportion of outpatient abdominal CT scans performed with and without contrast compared with scans performed with or without contrast, but not both. Both scans are typically not necessary, so the metric is commonly used to look for signs of potential overutilization.
To address this CMS measure, iOrder prevents potential overutilization and incorrect orders with order stoppages. Collaborative notes also keep patients safe. No more emails back and forth! Our notes system improves the continuum of care and increases patient safety.
OP-23: Head CT or MRI Scan Results
CMS Quality Measure OP-23: Head CT or MRI scan results measures head CT or MRI scan results for acute ischemic stroke or hemorrhagic stroke patients who received head CT or MRI scan interpretation within 45 minutes of ED arrival. iOrder flags the order for proper diagnosis and has a stat function that improves the workflow process. You can better prioritize scheduling, and no orders are missed, all within 45 minutes of arrival depending on how fast a radiologist can read the scan.
OP-29: Colonoscopy Follow-Up
CMS Quality Measure OP-29: Colonoscopy follow-up measures the percent of patients receiving appropriate recommendations for follow-up screening colonoscopies. If your organization is on a mission to improve colonoscopy screenings and follow-ups, iOrder routes results so every care provider can see information in real time. Other departments and services ancillary to the original diagnostic order can also be used as part of the follow up. This includes all imaging, lab work, etc.
These are just some of the ways iOrder can help improve your CMS quality star ratings. To learn more, contact us or request a free live demo today.