Burnout has been a hot topic in healthcare for many years, and we’ve covered the topic extensively in previous blog posts. When the topic of burnout comes up, people typically think of clinicians first. However, nurse burnout has become just as serious, if not more so than clinician burnout. With January 23rd-29th designated as National CRNA Week and the first-ever Ambulatory Care Nursing Week February 7th-13th, we’re focusing specifically on nurse burnout, highlighting key stats from recent surveys and looking at potential solutions.
How Bad is Nurse Burnout?
The first step to addressing nurse burnout is understanding just how bad it really is. According to a Medscape survey on nurse career satisfaction, at least 53% of nurses in each of the six nursing professions (CNS, CRNA, LPN, NM, NP, & RN) represented by the 10,500 respondents are “at least somewhat burned out.” To fully understand burnout’s seriousness, let’s take a look at what causes nurse burnout and the consequences it brings.
Causes of Burnout
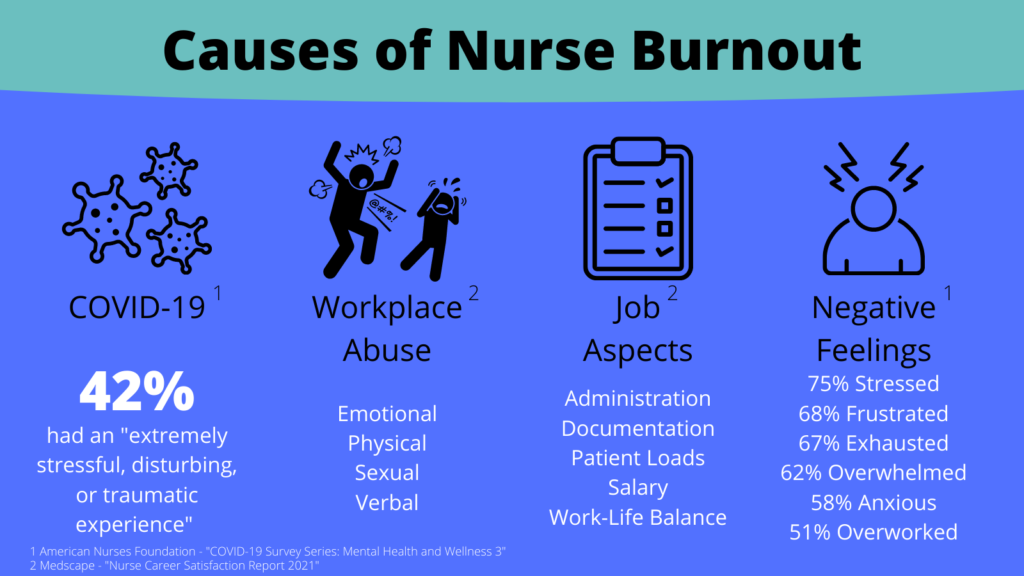
Nurses may experience burnout due to a variety of factors. Looking at data from several recent surveys on nurse burnout, there seem to be four major contributors:
- COVID-19
- Abuse in the workplace
- Certain aspects of the job itself
- Negative feelings
Let’s take a closer look at each of these burnout contributors.
COVID-19
The aforementioned Medscape report on nurse career satisfaction sheds some light on contributors to burnout. Unsurprisingly, the COVID-19 pandemic is at least partially to blame. At least 25% of nurses in each of the six nursing professions reported that the pandemic decreased their job satisfaction. NM’s and RN’s experienced the largest decrease in job satisfaction due to the pandemic – 41% and 40% respectively.
Additionally, a survey of 9,500 nurses published by the American Nurses Foundation in October 2021 found that 42% of respondents reported having “an extremely stressful, disturbing, or traumatic experience” to COVID-19. Of those 42%, more than half said that negative COVID-19 experience at least moderately bothered them in the following ways:
- Difficulty concentrating
- Feeling distanced/cut off from others
- Feeling irritable or having angry outbursts
- Feeling very upset when something reminded them of the experience, and
- Repeated disturbing thoughts, memories, or images of the experience
Workplace Abuse
In addition to the pandemic, respondents to the Medscape survey reported experiencing various types of abuse, including:
- Emotional – at least 31% in all 6 specialties
- Physical – about 20% of LPN’s, NP’s, & RN’s
- Verbal – at least 40%
- Sexual – 9-16%
While physical abuse was attributed mostly to patients, nurses reported experiencing significant amounts of emotional and verbal abuse from managers, coworkers, patients, visitors, and physicians alike. Sources of sexual abuse weren’t provided in the survey.
Specific Aspects of the Job
The Medscape survey also asked nurses about the least satisfying parts of their jobs, which could also contribute to burnout. The top 5 responses were:
- Administration/workplace politics
- Amount of documentation required to complete
- Lack of work-life balance
- Patient load/patient-to-nurse ratio being too high/not enough time to spend with patients
- Salary
Negative Feelings
The burnout contributors we’ve discussed so far can all lead to the fourth contributor: negative feelings. The American Nurses Foundation survey provided great insight into nurses’ feelings by asking the 9,500 respondents if they had experienced any of a multitude of positive or negative feelings in the past 14 days. The top 10 feelings experienced by respondents were all negative, and over half of the nurses reported experiencing 6 of those 10:
- Stressed – 75%
- Frustrated – 68%
- Exhausted – 67%
- Overwhelmed – 62%
- Anxious – 58%
- Overworked – 51%
The positive feeling experienced most by nurses was “grateful,” with only 38% of nurses experiencing this feeling. The next positive feeling on the list was “happy” – a mere 33%.
Consequences of Burnout
Now that we’ve discussed some of the causes of nurse burnout, it’s time to look at the potential consequences. As with clinician burnout, nurse burnout has consequences for nurses themselves, their coworkers, patients, and the healthcare organization as a whole.
Consequences for Nurses
The last contributor to burnout we discussed, negative feelings, is also one of the major consequences of burnout. In this way, it is compounding. Nurses experience these negative feelings, such as stress and frustration, as a result of burnout, which in turn exacerbates their burnout. This in turn leads to decreased satisfaction with their job and, most troubling for nurses themselves, mental health issues.
In fact, one-third of respondents in the American Nurses Foundation survey said they were “not emotionally healthy”. Furthermore, only 35% of nurses said they were emotionally healthy – the final third considered themselves neutral. Half of the respondents (21% “Yes” and 29% “Maybe”) said they may quit their job in the next 6 months, and the number one reason (47% of those who intended to quit) was “work is negatively affecting my health/wellbeing.” The next two reasons were insufficient staffing (41%) and “lack of support from employer during the pandemic” (31%). Side effects of burnout reported by nurses include:
- Sleep issues – 68%
- Overeating – 43%
- Relationship issues – 27%
- Oversleeping – 22%
- Alcohol consumption – 20%
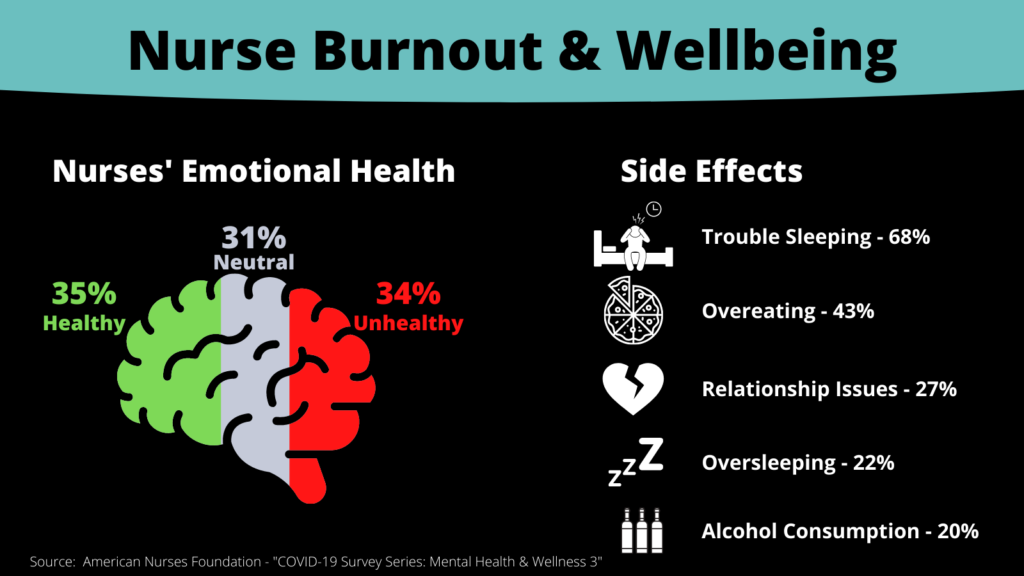
The negative feelings, decreased job satisfaction, poor emotional health, and potential of 50% turnover reported by nurses could lead to serious consequences for their coworkers, patients, and employers.
Consequences for Employers, Coworkers, and Patients
Burned out nurses could negatively impact their employers, coworkers, and patients in a number of ways. For one, nurses who are stressed out, frustrated, and tired may provide lower quality care to patients or call in sick/leave early to deal with their burnout symptoms. In a worst-case scenario, lower quality care could have serious health consequences for patients. Even in a best-case scenario, drop-offs in care can lead to a negative patient experience and could impact patient loyalty, creating a snowball effect culminating in revenue leakage for providers.
Similarly, nurse absenteeism puts more pressure on an already strained and possibly understaffed care team, which could lead to more burnout among nurses, clinicians, and other staff, compounding an already growing problem. In fact, healthcare staffing issues have become so serious in recent months that the U.S. government is investing $1.5 billion to combat the issue. Even worse than absenteeism is outright turnover. A recent survey found that turnover rate for RN’s alone was 18.7%. The same survey found that the average cost of RN turnover was $40,000, which could result in total nurse turnover costs of over $6 million for the average hospital.
Now that we’ve seen how bad nurse burnout is and the serious consequences it can lead to, let’s discuss what can be done about it.
What Can Be Done About Nurse Burnout?
As bad as burnout is among nurses, there are steps healthcare providers can take to mitigate the problem. The key is addressing the least satisfying parts of the job. As a refresher from the previous section, the five least satisfying of their jobs according to nurses in the Medscape survey are:
- Administration/workplace politics
- Amount of documentation required to complete
- Lack of work-life balance
- Patient load/patient-to-nurse ratio being too high/not enough time to spend with patients
- Salary
With these in mind, lets look at some measures that address each of these pain points, some of which can address multiple pain points at once.
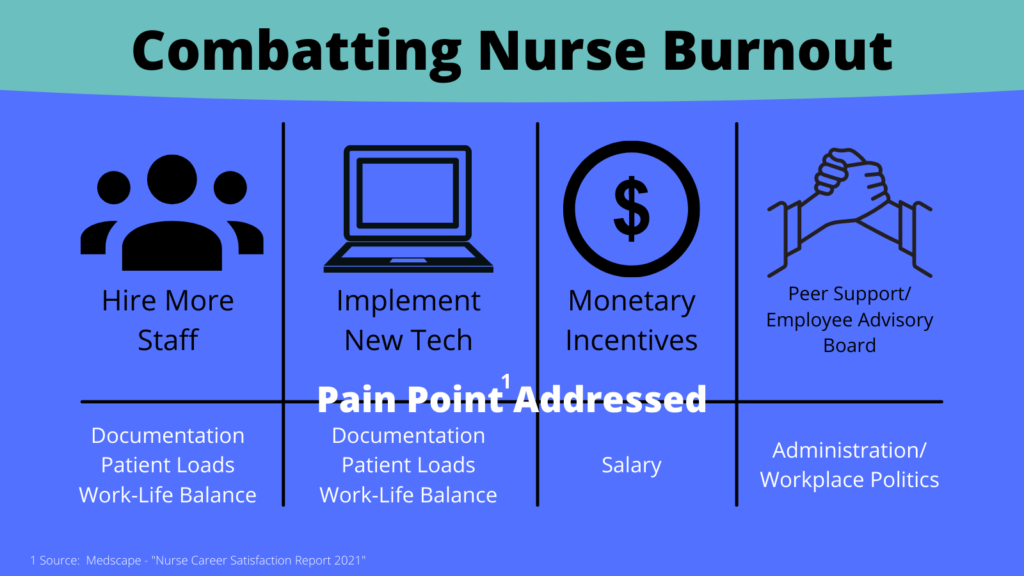
Hiring More Staff
Hiring more staff can address 3 of the least satisfying parts of nursing: the amount of documentation, lack of work-life balance, and the stresses of high patient loads. Based on HHS data posted January 6th, 2022, around 19% of all U.S. hospitals are critically understaffed. Hiring more staff can help reduce nurse workloads, such as the amount of time completing documentation, and help more nurses focus more on attending to patients. This can help lower the patient-to-nurse ratio and allow each nurse more time to spend with patients, improving the quality of care they provide (and thus improving the patient experience). Having more staff on hand can also help reduce individual staffing hours, promoting a better work-life balance for nurses and other staff.
Implementing New Tech
An alternative to hiring more staff is implementing new technology that can streamline workflows, eliminate menial tasks, and improve overall efficiency. As David Hancock, healthcare executive advisor at InterSystems puts it, “funds need to be focused on increasing productivity and patient safety.” Hancock also highlights the importance of interoperable tech – systems that safely and effectively share information with each other.
So what types of tech can help mitigate nurse burnout? Here are a few examples:
- Automated patient messaging platforms for patient notifications and appointment reminders
- Order management systems that produce digital patient orders with complete transparency
- Prior authorization assurance platforms that alleviate the burdens of the prior authorization process
- Self-scheduling solutions that empower patients to schedule their own appointments
There are other solutions that can help as well, particularly those that use AI or RPA (robotic process automation) to automate workflows. Of course, budget is always a concern when implementing new tech. For many providers, a hybrid approach of hiring more staff and implementing new technology may make the most sense. When it comes to funding, Hancock says that as IT solutions are moving to a more subscription-based model, operational expenditure should be the focus as opposed to capital expenditure.
For more examples of how tech can be used to combat healthcare staff shortages, check out our recent blog post.
Monetary Incentives
While it may be necessary to hire more staff, it’s equally important to retain the staff you already have. As we’ve already seen, salary and compensation is one of the top 5 least satisfying aspects of nursing and can lead to nurses quitting their jobs and sometimes the profession altogether. In fact, nurses are leaving their hospital jobs for travel nursing jobs that pay upwards of 5 times their current salary.
Straight up salary increases are one way to use monetary incentives to retain staff, but could also be very costly. Another incentive some hospitals have used is offering more money for extra shifts. Other incentives hospitals are turning to include pay-on-demand, which allows employees to take a paycheck the day after they work a shift, and student loan repayment programs. If you’re interested in offering monetary incentives as a nurse retention tactic, consider administering an internal survey asking nurses what type(s) of incentive(s) appeal to them most.
Peer Support Groups and Employee Advisory Boards
The number one job-related pain point according to nurses is administration/workplace politics. Tackling this pain point isn’t as straightforward as hiring more staff, implementing new technology, or offering monetary incentives. According to the Medscape survey on nurse job satisfaction, managers and administration were leading sources of both emotional and verbal abuse for several nursing groups.
This type of toxic work environment cannot and should not be tolerated. An adage that has become increasingly popular over the years is “people quit bosses, not jobs.” It’s not surprising that administration and workplace politics is the least satisfying part of nursing for so many in the profession. To combat this issue, healthcare providers should consider creating employee advisory boards that can provide feedback on the workplace environment and hold management (and other employees) in check. Peer support groups can also give employees an avenue to vent and relieve stress.
When nurses know their employer has their back and their best interest at heart, it can go a long way in reducing, and maybe even preventing, burnout.
We’re Here to Help
We’ve discussed some of the causes of nurse burnout, as well as its consequences. We’ve also discussed several ways healthcare leaders can combat nurse burnout. Now, let’s discuss how we can help.
At iPro Healthcare, we offer a solution that not only creates a better experience for physicians and patients, but can also make nurses’ jobs easier: iOrder ambulatory order management. With our iOrder solution, you can generate a digital patient order with complete transparency, eliminating faxes and lost orders. Plus, iOrder is interoperable with the EHR and can be integrated with other third-party applications. Each order is validated for order accuracy, and an integrated Clinical Decision Support Mechanism (qCDSM) ensures PAMA compliance and maximizing reimbursements.
All of this ensures patient order information is accurate and easily accessible. When delivering results to patients over the phone or answering questions about an upcoming exam, iOrder ensures nurses have all the information they need. iOrder can also reduce workloads by sending patients automated appointment reminders, links to procedure-specific instructions and videos, and navigation assistance. We also offer prior authorization services that take the burden of tracking prior authorizations off of nurses and other staff. Ultimately, iOrder reduces human error and frees up nursing staff to spend more time with patients and less time dealing with documentation.
If you’d like to learn more about iOrder, contact us today or schedule a live demo.




