2020 was the most challenging year most healthcare leaders and workers have ever experienced. The COVID-19 pandemic reshaped every aspect of life and changed the world as we know it. On top of the pandemic, 2020 was also an election year. As such, healthcare executives not only have to stay on top of the latest COVID-19 developments, but also incoming policy changes from the Biden administration. Furthermore, executives must ensure their facilities are prepared for PAMA regulations that are finally going into full effect, with reduced Medicare reimbursement rates in 2022. As always, executives must also stay up-to-date on emerging technologies to meet the ever-evolving challenges in healthcare. Finally, leaders should keep their staff’s wants and expectations top of mind.
Leadership in healthcare is always challenging, but perhaps never more than in 2021. In this post, we’ll discuss some tips for leading in the new year, from managing the ongoing COVID-19 pandemic, to navigating policy changes, staying up-to-date on the latest healthcare technologies, and meeting the expectations of clinical staff.
Managing COVID-19
Even though 2020 is behind us, COVID-19 is not. In fact, health systems across the country could be faced with their most challenging task yet in the coming weeks due to an expected surge in COVID-19 cases from the holiday season. Healthcare leaders will be forced to make tough decisions, such as the recent directive in Los Angeles County to EMS teams to not transport patients with low survival chances to local hospitals. As of January 2nd, LA County has over 800,000 cases of COVID-19, double the amount of cases on November 30. Furthermore, over 7,000 patients are currently hospitalized. With limited capacity, healthcare leaders have had to result to drastic measures, such as the previously mentioned EMS directive and opening up triage centers in church gymnasiums. Lessons learned from the first wave of the pandemic will prove useful in combatting this second wave.
Vaccine Distribution
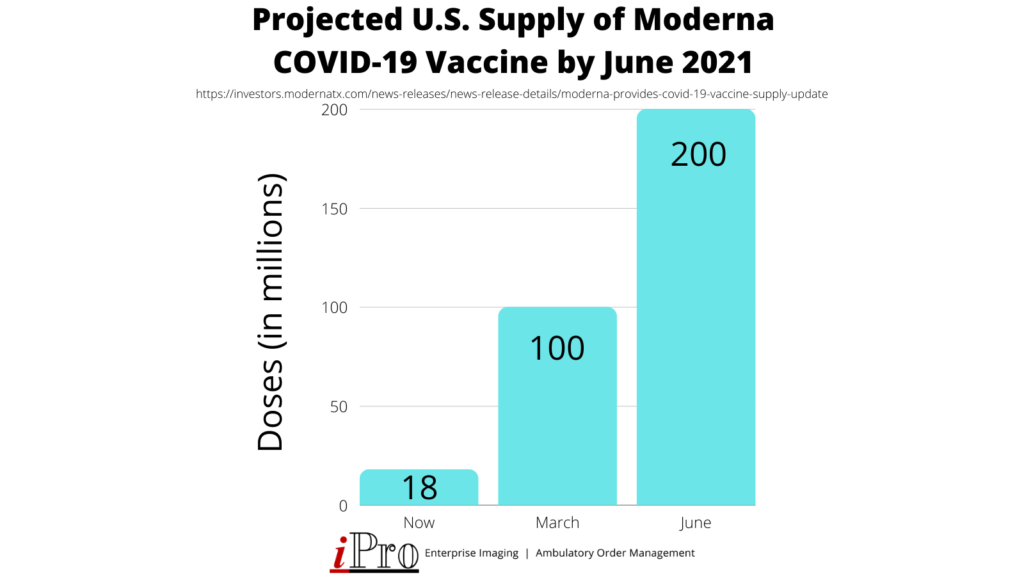
Fortunately, vaccine distribution began in December and will continue to roll out over the coming months. So far however, the rollout has been slower than expected, with only an estimated 4.5 million doses administered out of nearly 15.4 million distributed across the country. Officials had hoped to have administered 20 million doses by New Year’s Day, but only about 23% of that goal was reached, which means herd immunity is still months away. Fortunately, Moderna announced on January 4th that they will be ramping up production and expect to have 100 million doses of their vaccine distributed by March. By June, they project the supply will double to 200 million, and hope to have between 600 million and 1 billion doses by the end of 2021.
Healthcare leaders will need to stay on top of the latest vaccine developments and coordinate the vaccine rollout at their facilities throughout the year.
Healthcare Policy and Regulation Changes
COVID-19 has been a major catalyst for change in its own right. However, the results of the 2020 U.S. presidential election are sure to bring about more major changes to healthcare. In the next section, we will examine what healthcare leaders should expect from the Biden-Harris administration, as well as the latest on PAMA, the Protecting Access to Medicare Act.
Biden Administration Healthcare Policy
As expected, much of the Biden administration’s focus upon taking office will be the COVID-19 pandemic. One of the first actions the new president plans on taking is invoking the Defense Production Act to ensure “the personal protective equipment, the test capacity and the raw materials for the vaccines are produced in adequate supply,” according to Dr. Celine Gounder, a member of Biden’s COVID-19 advisory board. This will allow vaccine manufacturers such as Pfizer and Moderna to have priority in sourcing the materials they need to streamline vaccine production. President-elect Biden will also establish a COVID-19 task force to oversee vaccine distribution and a national vaccination campaign.
In addition to managing the COVID-19 crisis, Biden also placed a strong emphasis on shoring up the Affordable Care Act during his election campaign. Biden’s plans for the ACA aren’t set in stone, but discussions have included:
- Reopening insurance marketplaces with extended sign-up periods as opposed to the six-week periods under the Trump administration
- Restoring millions in federal funding cut by the Trump administration for a national advertising and outreach campaign encouraging people to sign up
- Establishing a public option alternative to private insurance plans
- Lowering Medicare eligibility from age 65 to 60
- Expanding Medicaid eligibility in a dozen states that have not done so under existing ACA provisions
It’s worth noting that none of these proposed changes are officially decided upon, and most would require congressional approval. Still, healthcare leaders should be aware of them and stay up-to-date on the latest news involving the Affordable Care Act.
Protecting Access to Medicare Act (PAMA)
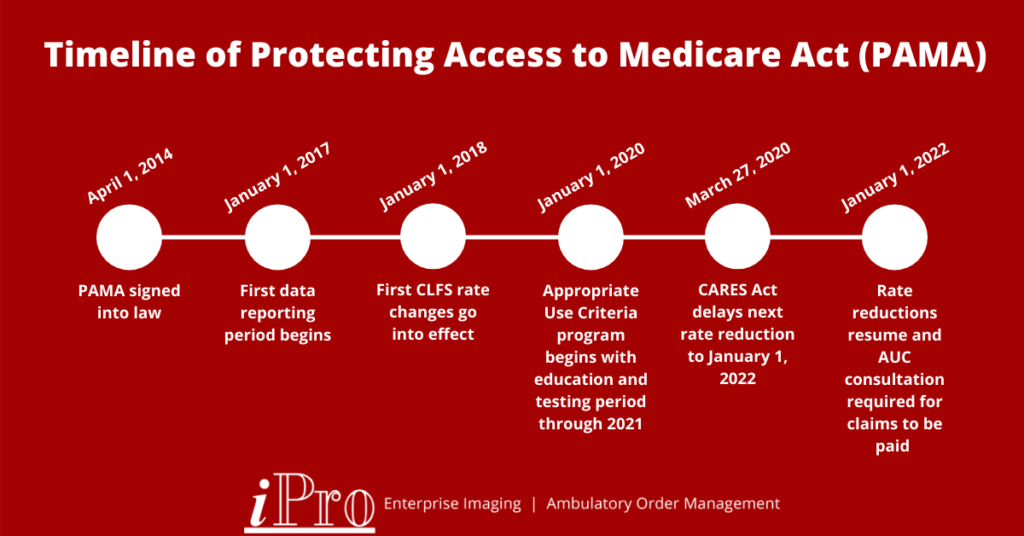
In addition to following the Biden-Harris administration’s healthcare policy, healthcare leaders should be familiar with the Protecting Access to Medicare Act, or PAMA, and ensure their facilities are prepared for when the act is fully implemented on January 1, 2022. Signed into law in 2014, PAMA made significant changes to Medicare reimbursement of Clinical Diagnostic Laboratory Tests (CDLTs). Under PAMA, applicable institutions must report private payer data to CMS (Centers for Medicare & Medicaid Services). CMS will use this data to reduce Medicare reimbursement rates for CDLTs to ensure the rates are more in line with those paid by private insurers.
Due to the COVID-19 pandemic however, some of the program deadlines have been extended. Most importantly, there will be a 0% reduction in reimbursement rates for 2021. Instead, reductions will resume on January 1, 2022 with a reduction cap of 15% through 2024. The data reporting period of January 1, 2022 through March 31, 2022 will be based on the original data collection of period from January 1, 2019 through June 30, 2019.
In addition to the data reporting requirements, PAMA also requires physicians consult a quality Clinical Decision Support Mechanism (qCDSM) to ensure Appropriate Use Criteria (AUC) when ordering advanced imaging exams. This helps reduce billing errors by ensuring the correct exam is ordered for each patient. The AUC program went into effect on January 1, 2020 with an education and testing period running from January 1, 2020 through 2021. During this time, physicians should become familiar with AUC and qCDSMs when ordering advanced imaging exams. Beginning January 2022, Medicare claims that do not have proof of the ordering physician’s AUC consultation through a qCDSM appended to them will not be paid. See the timeline below for a simplified overview of PAMA and the AUC program.
For more info on PAMA and the AUC program, check out the CMS FAQ page or visit nationaldecisionsupport.com.
Emerging Technologies
One of the most important responsibilities of healthcare leaders is evaluating emerging technologies. Implementing new technologies can help comply with new regulations, such as PAMA, and introduce new revenue streams, such as telehealth services. Health IT Answers recently asked several healthcare industry experts about their health IT predictions for 2021. Denny Phillips, President and CEO of iPro, Inc had this to say:
“Healthcare IT departments of the future will need to focus on three initiatives to help their facilities thrive: transformative technology, a patient-centered approach to care, and service delivery excellence.”
Denny Phillips, President & CEO, iPro, Inc
If there’s a silver lining to the COVID-19 pandemic, it’s that it has ushered in a wave of technological advances that greatly benefits the healthcare industry. In this section, we’ll look at some technologies hospital executives should consider implementing, whether they be for their hospital command center, digital front door, or general facility improvements.
Artificial Intelligence and Machine Learning
Recent years have seen great advancements in artificial intelligence and machine learning. Artificial intelligence, or AI, has a variety of applications in healthcare, such as wearable devices, predictive analytics, and even detecting diseases such as COVID-19. AI helps provide better care and a better patient experience, providing the hospitals that incorporate it a competitive advantage. AI may soon not be a way for hospitals to differentiate themselves from competitors, however – it may become expected by patients. As more and more consumer devices incorporate AI and machine learning, it “will challenge traditional healthcare organizations to compete with emerging retail and virtual providers in ways we have not experienced before,” according to Eric Yablonka, CIO and Associate Dean of Technology and Digital Solutions at Stanford Health Care and School of Medicine.
Order Management Software
Order management software, like our iOrder solution, can help revolutionize your ambulatory care department. iOrder eliminates faxes and time spent on hold by producing an electronic order with complete transparency. This helps streamline workflows and improves efficiency. Plus, iOrder is complete with an integrated qCDSM mechanism, ensuring the correct order every time in compliance with PAMA’s Appropriate Use Criteria requirements. Implementing an order management solution is a great way to improve efficiency and patient experience and increase reimbursements.
Remote Patient Monitoring Devices
Remote patient monitoring saw a boom in adoption last year due to the COVID-19 pandemic. Providers needed a safe way to monitor patients while minimizing the risk of virus transmission. Remote patient monitoring devices can be used for countless applications, including monitoring heart rate, measuring blood pressure, and even analyzing nutrition information from patient’s meals. If you’re interested in implementing a remote patient monitoring program at your facility, check out these tips from the Medical Group Management Association (MGMA).
Telehealth Platforms
Telehealth has been a literal lifesaver during the COVID-19 pandemic. The practice had faced slow adoption rates in the few years prior to 2020, but the outbreak of the pandemic forced providers to pivot. The first quarter of 2020 saw a 50% increase in telehealth visits over the same period in 2019. 93% of these telehealth encounters were for conditions other than COVID-19. One thing’s for sure: telehealth is here to stay, and healthcare leaders should stay up-to-date with its latest developments in order to provide the best care for their patients.
Clinical Staff Wants and Expectations
Healthcare leaders have a lot to think about in 2021. From managing the ongoing COVID-19 pandemic, to navigating inevitable policy changes, to evaluating the latest tech, it can seem overwhelming. Even with all these issues top-of-mind, healthcare leaders can’t lose sight of one of their most important responsibilities: personnel management. In fact, listening to medical personnel on the frontlines is more important than ever. Healthcare leaders should not only be concerned with how personnel is feeling, but also what they expect from leadership and solutions they believe would improve the work environment. Becker’s Healthcare recently spoke with frontline medical staff across the United States and asked them what they wanted their leaders to know. We’ve summarized their responses below:
How are they feeling?
- Anxious, depressed, fearful, lonely, and tired due to the pandemic
- Appreciative for empathy and compassion shown by leaders
- Encouraged by a sense of teamwork and togetherness from peers and leadership
- Rewarded for taking care of patients and being recognized and appreciated by leadership
- Well-prepared as a result of leadership’s commitment to securing PPE and innovative technology
What do they want?
- Access to COVID-19 testing for their families
- Expanded emphasis on employee well-being
- More opportunities for training and development
- Ongoing improvements to communication and information relay
- Protocols for providing immediate resources for staff and families that have experience trauma
While these sentiments offer some insight into how medical staff may be feeling, every facility is different. The best way to know how your staff is feeling and what they want is to ask them. Consider administering a survey, or use this AMA survey for gauging burnout at your facility.
Leading in the New Year
2020 was the most challenging year most healthcare leaders have ever faced. One positive from 2020 is that it provided many lessons learned that can help executives lead through 2021 and beyond. While new issues are sure to arise, some of the most pressing inlcude:
- The ongoing COVID-19 pandemic
- New healthcare policies and initiatives from the Biden-Harris administration
- Emerging technologies
- Addressing medical staff wants and expectations
As healthcare leaders navigate these challenges and unforeseen ones sure to arise, they don’t have to do it alone. Peer groups can be a valuable source of support and resources. Partnering with the right vendors can also make a world of difference. At iPro, our vision is to help every client be successful with our software solutions through quality services & support. We’ve been helping our clients achieve their goals since 1998. If you’d like to learn more about how we work with you every step of the way, check out our partnership lifecycle diagram or contact us today.




