This time last year, we took a look at some of healthcare’s biggest fears and how to fight them. With Halloween right around the corner, it’s time for a sequel. In this edition, we’ll look at 3 new fears, as well as an old one that’s still lurking around like a horror movie villain…
Fear #1: PAMA
The Protecting Access to Medicare Act, or PAMA, has been lurking in the background since 2014, threatening payment reductions for Medicare claims submitted without proof of clinical decision support consultation. PAMA has been in an educational and testing phase for nearly a decade, giving providers ample time to get familiar with qualified clinical decision support mechanisms (qCDSMs). It’s also given them plenty of time to procrastinate, with PAMA’s penalty phase being delayed again and again. As of now, the Centers for Medicare and Medicaid (CMS) says it is “unable to forecast when the payment penalty phase will begin.”
However, this doesn’t mean the threat of PAMA and denied claims has gone away. CMS still plans on implementing the penalty phase sometime in the future. This means providers should take advantage of the extra time to become acquainted with qCDSMs and the clinical decision support process. This initiative can take months or even a year or two, so providers and health systems shouldn’t wait until it’s too late to start implementing clinical decision support and getting comfortable using it. Fight the lingering fear of PAMA and reduced reimbursements by being proactive about clinical decision support.
Fear #2: Disasters
Hurricane season is upon us. Hurricane Ian made landfall at the end of September and forced health systems in Florida and South Carolina to take emergency action. As with past hurricanes, Ian created several challenges for health systems, including:
- Damage to facilities
- Loss of power
- Evacuating patients
- Supply chain delays
Like hurricanes, other natural disasters such as tornadoes and earthquakes can have devastating effects on health systems. To fight the fear of disasters, it’s important for health systems to have an Emergency Action Plan in place for each type of natural disaster they may encounter. Additionally, a disaster recovery plan should be agreed upon to mitigate downtown and loss of data, and to ensure operations can get back up and running as quickly as possible. In healthcare, every second counts. Finally, partnering with software vendors who offer 24/7 support is crucial to ensure you have the help you need in the event of a disaster.
Read our blog on how hospitals have responded to disasters for more tips on preparing for, responding to, and recovering from various disasters, including pandemics and cyber attacks.
Fear #3: Healthcare Disruptors
A growing fear over the last few years is that of healthcare disruptors: companies that haven’t traditionally provided healthcare services that have begun entering the market. Healthcare disruptors include big-box retailers, tech giants, and more, such as:
- Amazon
- Apple
- CVS
- Walgreens
- Walmart
The consumer-facing companies are disrupting the traditional healthcare space by offering their own health services, including brick-and-mortar clinics and one-stop-shops for health services from primary care to imaging. Additionally, tech giants like Google and Apple are working on innovative tech solutions to improve EHR’s, the patient experience, and more. These companies pose a threat to traditional healthcare providers in three ways:
- Service disruption
- Tech disruption
- Financial disruption
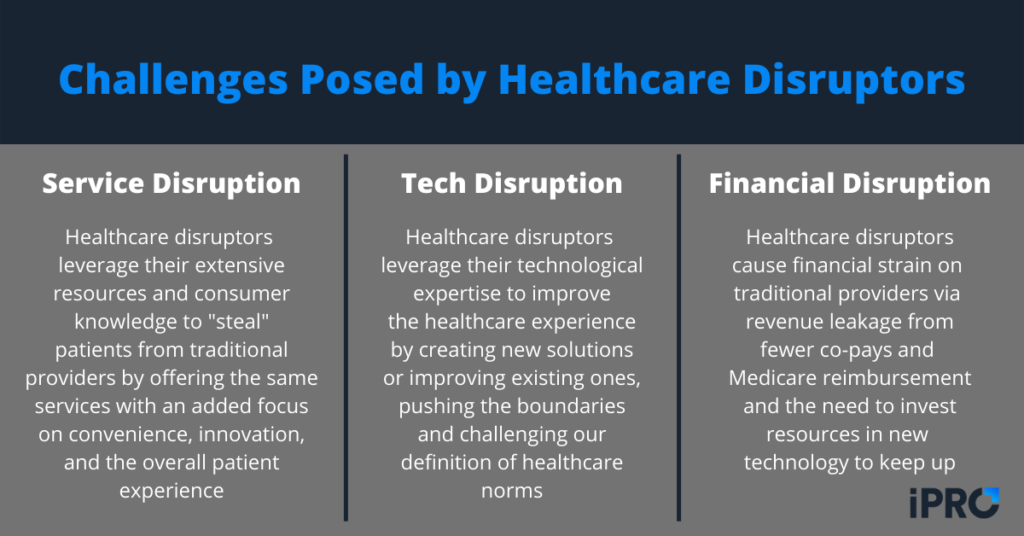
By leveraging their reputation, customer service experience, and tech advantages, healthcare disruptors can lure patients away from traditional providers. To fight the fear of healthcare disruptors, traditional providers should focus on strengthening their relationships with referring providers and improving the patient experience.
For a more in depth look at how healthcare providers can disrupt the disruptors, read our blog.
Fear #4: Burnout and Turnover (Again…)
The final fear we’ll discuss is an old one that just won’t go away: burnout. Burnout has been a persistent challenge in healthcare for some time now, made worse by the COVID-19 pandemic. Burnout can lead to several negative outcomes for patients, providers, and health systems, including:
- Employee absences
- Adverse coping mechanisms (drugs, alcohol, junk food)
- Adverse health outcomes for patients
- Employee turnover and staffing issues
- Loss of revenue and reputation for hospitals
There are many causes for and contributors to burnout. The AMA lists the following as some of the top contributors:
- Work overload
- Lack of control
- Insufficient rewards
- Breakdown of community
- Sense of unfairness
- Conflicting values
Fighting the fear of burnout and resulting turnover can be complex. Since there are many causes for burnout, there’s not a one-size-fits-all solution. Generally, burnout reduction initiatives should focus on:
- Reducing workloads
- Streamlining workflows
- Collecting feedback from healthcare workers
- Promoting mental health
- Offering competitive compensation
- Improving work-life balance
For tips on attracting and retaining top talent, check out these 14 benefits health systems offer employees.
Let’s Stick Together
Healthcare can be a scary place with various fears lurking around every corner. Fortunately, you don’t have to fight those fears alone. At iPro Healthcare, we’ve been helping hospitals, health systems, and imaging centers face their fears and conquer their challenges for nearly 25 years. Our flagship ambulatory referral management solution, iOrder, helps address all the fears we’ve discussed so far.
iOrder generates an electronic patient order with complete transparency and validation. An integrated clinical decision support mechanism (qCDSM) ensures PAMA’s Appropriate Use Criteria mandate is satisfied. This not only improves order accuracy and patient safety, but it also minimizes claim denials and maximizes reimbursement.
Improved accuracy and safety also helps improve the patient experience and foster patient loyalty, which is key to competing with healthcare disruptors. Patient experience and loyalty are further strengthened through iOrder’s patient engagement features, including:
- Appointment reminders via text
- Procedure-specific instruction videos that ensure patients are properly prepared
- GPS navigation assistance
These features, combined with integrated prior authorization assurance help reduce workloads, streamline workflows, and mitigate burnout. Clinical staff have more time to spend with patients instead of being bogged down with administrative tasks. Plus, iPro support is ready 24/7 to help in the event of a disaster.
If you’d like to learn more about how we can help you fight your healthcare fears, contact us today or schedule a free iOrder demo.