The world of healthcare can be a scary place for both patients and providers. From the ever-present threat of cyber attacks to provider burnout and turnover, healthcare leaders and workers face a multitude of fears everyday. On top of that, there are also financial fears to consider. The COVID-19 pandemic has only compounded these fears and introduced fears of its own. In this blog, we’ll look at some of the biggest healthcare fears and how healthcare leaders can fight them.
Fear #1: COVID-19
Obviously the biggest fear in the healthcare world right now is COVID-19. The pandemic has been pushing healthcare to the brink for a year and a half, and though vaccines have proven to be an effective weapon against the virus, we still have a ways to go. As of this writing, daily COVID-19 cases and deaths in the U.S. are on the decline, but 70 million eligible Americans remain unvaccinated. This sombering fact has healthcare leaders preparing for the next wave even as the current seems to be dying down.
There is cause for optimism, however. For starters, pharmaceutical giant Merck has announced a new pill that it says cuts COVID-19 hospitalizations and deaths in half when taken early in the infection. The pill is currently experimental and is awaiting FDA approval. If approved, it can be a game changer. Coupled with increased vaccination rates, incremental as they may be, we may soon have the one-two punch needed to effectively knock out COVID-19.
In addition to the promising pill and increased vaccination rates, University of Maryland researchers are currently developing new PPE, funded by the CDC. The new type of mask is meant to be more comfortable than the widely-used N95 masks. This new mask features goggles fitted with a HEPA filter that keeps airborne particles out. The device can be calibrated for a more comfortable fit due to a built-in sensor that measures micro pressure, CO2, humidity, and temperature. It can also be sterilized with UV light.
While COVID-19 is a formiddable foe, the tide may finally be turning in favor of humanity.
Fear #2: Cyber Attacks
Cyber attacks are another major healthcare fear. Healthcare organizations provide a prime target for cyber criminals for three reasons:
- They are perceived to have the financial means to pay ransoms
- They would need to act quickly in the event of a cyber attack in order to keep critical operations running with patients’ health at risk
- Their fast-paced environment can lead to lapses in cybersecurity best practices, such as locking computers
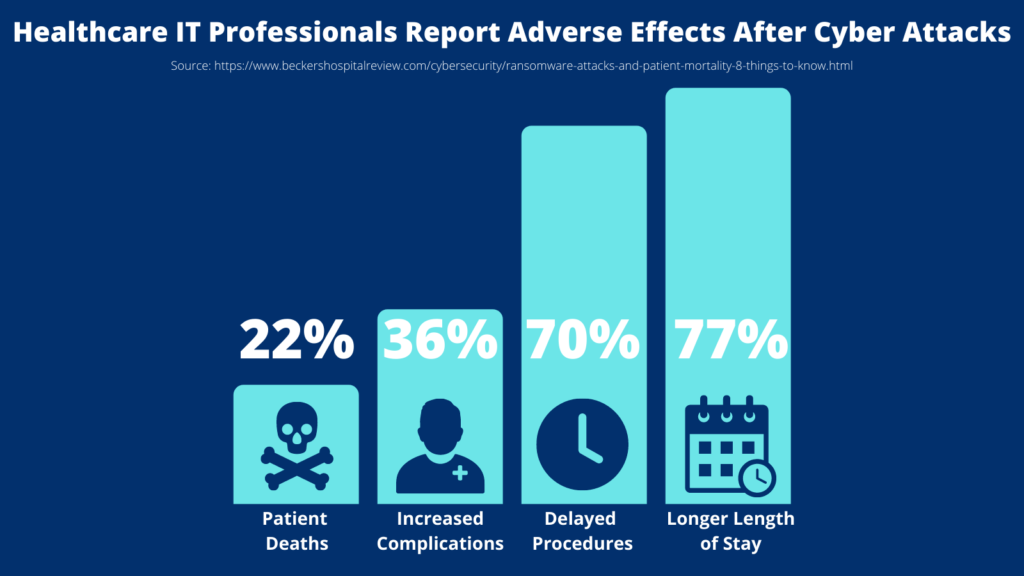
Healthcare providers often feel like they have no choice to pay ransoms when critical data and systems are compromised. If staff is locked out of their computers for extended periods, patient care can be delayed. In fact, a recent report by the Ponemon Institute found that 22% of healthcare facilities experienced excess patient deaths following ransomware attacks. Respondents to the Ponemon Institute survey also reported the following adverse effects of cyber attacks:
- Longer length of patient stays (77%)
- Procedure and exam delays leading to poor health outcomes (70%)
- Increased complications from medical procedures (36%)
This is why having proper cybersecurity protocols in place is essential. From a high level perspective, three keys to cyber vigilance are:
- Knowing the different types of cyber attacks (e.g. phishing, ransomware, etc.)
- Proactive preparedness (Anti-virus software, cybersecurity awareness training, etc.)
- Knowing how to respond when a cyber attack occurs (shutting down computers, backing up data, etc.)
For a more in depth overview of how to remain cyber vigilant even during a pandemic, check out our blog on the topic. The unfortunate reality of cyber attacks is that they’re likely going to cost providers one way or another: providers will be forced to pay a ransom in the event of a cyber attack or they will need to invest more resources in cybersecurity prevention and response measures, such as clinical communication and collaboration platforms that can provide a secondary communication conduit in the event an EHR is compromised. This leads to our next healthcare fear: financial issues.
Fear #3: Financial Issues
Financial issues are also a major fear for healthcare leaders. As we mentioned in the previous section, many providers are committing more resources to cybersecurity. The pandemic has put a major strain on hospital finances, and while revenues have been recovering from 2020 levels, the Delta variant is hindering that recovery. This means hospital executives must carefully decide which projects in which to invest and which ones to put on hold. A major factor contributing to financial strain is staff burnout and turnover, which we’ll cover more in depth in the next section. Staffing issues affect the bottomline in two main ways: decreased procedure volumes due to staffing shortages and increased labor costs as providers are forced to raise salaries and offer bonuses to attract and retain staff.
In our blog post “6 Ways to Recover Healthcare Revenues and Stop the Leaks,” we discussed the following tactics healthcare leaders can use to address financial issues:
- Encourage patients that it’s safe to seek treatment
- Engage patients with a strong digital presence, such as a digital front door strategy
- Enhance offerings to maintain a competitive advantage, foster patient loyalty, and attract new patients
- Enlarge your referral base
- Minimize claim denials to maximize reimbursements
- Mitigate burnout
Check out that blog post for a deep dive on revenue recovery tips.
Fear #4: Provider Burnout and Turnover
The final fear we’ll discuss is provider burnout and turnover. While the pandemic has undoubtedly made burnout worse, 79% of physicians reported their burnout started before the pandemic according to a Q1 Medscape report. Nurses are also experiencing high levels of burnout, with 66% saying they’ve considered leaving the profession as a result of their pandemic experiences. A recent survey by the American Psychological Association found that 2 in 5 American workers plan to change jobs in the coming year. With healthcare institutions already facing staff shortages, this is especially concerning. Vaccine mandates have added to staff turnover as hundreds and even thousands of healthcare workers have either resigned in protest or been terminated for noncompliance. Some health systems have even resorted to offering large sign-on bonuses and on-the-spot job offers to attract new employees.
So, how can we fight burnout and turnover? It starts with improving mental health and well-being. Steps that can be taken to improve mental health and well-being include:
- Reducing workloads and streamlining workflows
- Investing in technology that makes staff’s jobs easier
- Providing access to mental health resources and support programs
- Giving providers more control and autonomy
- Encouraging time off
- Educating staff on how proper financial planning can relieve stress
If healthcare leaders didn’t already know, they’re finding out now that their employees are their most valuable resource. Losing them could be catastrophic, which is why mitigating burnout and turnover is crucial.
Fighting The Fears Together
Patients and providers both have a multitude of healthcare-related fears, with COVID-19 likely taking the top spot for both at the moment. Cyber attacks are also highly concerning for both patients and providers. In addition to these two pressing concerns, healthcare leaders must also deal with the fears of financial issues and staff burnout and turnover.
We’ve looked at measures healthcare leaders can take to fight each of these fears. At iPro Healthcare, we’re here to help you fight those fears together. Our flagship, award-winning ambulatory order management solution, iOrder, helps fight many of the healthcare fears we’ve discussed in this blog by:
- Generating an electronic medical order with complete transparency
- Offering a secure, HIPAA-compliant messaging and alert system
- Eliminating CPT/ICD-10 code mismatches and complying with PAMA via an integrated Clinical Decision Support Mechanism, thereby minimizing claim denials
- Reducing clinical workloads and streamlining workflows by eliminating faxes, back-and-forth phone calls, and on-hold time
If you’d like to learn more about iOrder, watch the short video below or contact us today.




