National Doctor’s Day is March 30th, and physicians all over will be celebrated with hashtags and supportive social media posts. While that’s nice and may boost morale a bit, those gestures may come across as hollow and performative if they’re not backed up with real action. To truly honor physicians and other clinicians this National Doctor’s Day, consider making a commitment to addressing a major problem many doctor’s face: physician burnout.
We recently took a deep dive into the state of nurse burnout; now it’s physicians’ turn. Read on to learn about the state of physician burnout in 2022 and how it’s changed over the years, COVID-19’s effect on physician burnout, and ways to combat it.
Physician Burnout Over the Last Few Years
Physician burnout has been growing over the last several years. Medscape has been reporting extensively on burnout during this time with their annual “Medscape National Physician Burnout & Suicide Report,” which surveys over 12,000 physicians across numerous specialties. To understand how the problem has changed year-to-year, let’s compare some stats from Medscape’s 2021 and 2022 reports (data presented in the reports was collected in 2020 and 2021 respectively).
Burnout in General
In 2021, Medscape found that 42% of physicians were burned out. This was already a staggering number. However, burnout affected even more physicians over the course of last year, with 47% of physicians reporting burnout in the 2022 report. Burnout among both genders rose 5% from 2020 to 2021, from 36% to 41% in men and 51% to 56% in women. While this 5% increase for both genders represented a larger percentage increase in burnout among men than women (14% vs 10%), female physicians are still experiencing burnout at a higher rate.
Burnout is also having a bigger impact on physicians’ lives than it was in 2020. 54% of physicians said burnout has a “strong/severe” impact on their life in 2021, compared to 47% in 2020. Further, the percentage of physicians reporting burnout having only a “moderate” or “little to no impact” on their lives decreased in both categories (24% to 22% and 29% to 24% respectively). Essentially, the percentage of physicians reporting a “strong/severe” impact on their lives (47% in 2020 to 54% in 2021) flipped the percentage of those reporting “moderate” or “little to no” impact (53% in 2020 to 46% in 2021).
Contributors and Causes
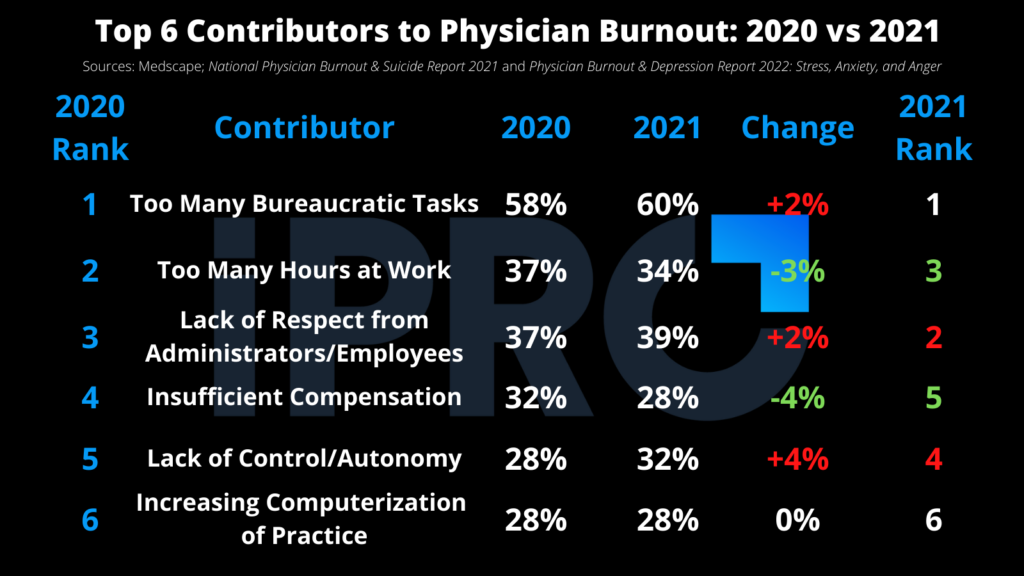
The top 6 contributors to burnout remained the same in both reports. However, there was some shuffling in the rankings, and half of those contributors saw increases in the percentage of physicians attributing them to burnout. The table below shows these top 6 contributors to burnout and how they changed from 2020 to 2021.
While these aspects of physicians’ jobs significantly contribute to burnout, the increase in the number of physicians experiencing burnout and its severity is likely due to a much bigger issue, which you’ve probably guessed by now…
COVID-19’s Effect on Physician Burnout
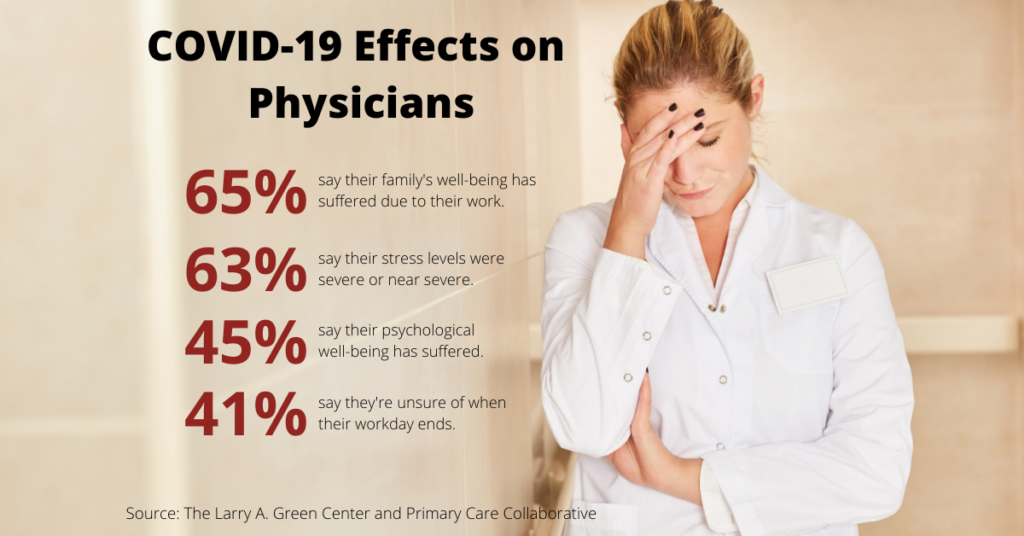
The COVID-19 pandemic is the most likely culprit for the rise in burnout and its severity. At the height of the pandemic’s onset, Primary Care Collaborative and the Larry A. Green Center conducted a survey gauging how the pandemic was affecting physician burnout. Key findings from the survey, fielded June 12-15 2020, include the following:
- 44% of physicians said their personal burnout was at an all-time high
- 45% of physicians said their psychological well-being had suffered
- 63% of physicians reported severe or near-severe stress levels over the past 4 weeks prior to the survey
- 65% of physicians said their families’ well-being had also suffered as a result of their work
While 79% of physicians in Medscape’s 2021 report said their burnout began before the COVID-19 pandemic, the pandemic has certainly made it worse. In that same report, physicians reported COVID-19 had significantly impacted their worklife happiness. 69% of physicians reported being happy (answer choices “somewhat happy” and “very happy”) with their worklife prior to the pandemic, while only 49% were happy at the time of the survey when the pandemic was in full swing. The number of physicians reporting being unhappy (“somewhat unhappy” and “very unhappy”) ballooned from 19% pre-pandemic to 34% during. These answers remained largely the same in the 2022 report.
Ways to Combat Physician Burnout
Now that we’ve seen how severe physician burnout is, let’s look at some ways to combat it. Based on a study conducted in 2019, the National Academy of Medicine recommended six system-wide actions healthcare providers should take to prevent or reduce burnout:
- Create positive work environments
- Create positive learning environments
- Reduce administrative burden
- Enable technology solutions
- Provide support to clinicians and learners
- Invest in research
Creating positive work and learning environments should be the first priority in providers’ burnout prevention efforts. This can be done in a variety of ways as long as the focus is on making physicians’ job easier and less stressful and ensuring they have adequate resources for support. The other four recommended actions all help create this positive environment, especially actions 3-5.
Reducing administrative burden and enabling technology solutions go hand-in-hand. While technology can be a contributor to burnout (such as too many hours spent in the EHR), the right tech can mitigate it. Tech that reduces workloads and streamlines workflows, such as ambulatory order management solutions and Clinical Decision Support Mechanisms (qCDSM’s) can mitigate and prevent burnout by eliminating time-consuming steps in daily workflows.
For instance, our iOrder ambulatory order management solution generates a digital patient order and eliminates the need for duplicate data entry and back-and-forth phone calls. Trimming 5 to 10 minutes off every outpatient order can result in hours of reduced work each week. Another great way to reduce administrative burden is outsourcing the prior authorization process to a third-party specialist. We’ve partnered with Auth-Net, a leading prior authorization services provider, to offer integrated prior authorization assurance with iOrder. This frees up physicians and other clinical staff to focus on patients as opposed to tracking the status of prior authorizations.
Finally, providing avenues of support for clinicians, such as peer-to-peer support groups and counseling services promotes a positive work environment. Continual investment in research on burnout, such as employee well-being surveys, helps providers know how their burnout prevention initiatives are working and what they can do better.
For tips on how to track your progress on preventing and mitigating burnout, checkout this guide by the American Medical Association.
We Stand with Physicians
At iPro Healthcare, we strive to make the healthcare experience better for patients, providers, and physicians. That’s why we created iOrder. Our award-winning ambulatory order management platform helps reduce burnout in several ways, including:
- Reducing workloads and streamlining workflows by eliminating faxes and duplicate entry
- Providing physicians with peace of mind through Clinical Decision Support and order validation
- Generating digital patient orders with complete transparency for easily tracking progress
To learn more about how iOrder can help in your burnout reduction efforts (and increase your bottom line), request a free live demo today.




